Sharp foreign bodies in GI tract
by Julien Puylaert and Frank Zijta
Amsterdam UMC and Haaglanden MC, The Hague
Publicationdate
This is an overview of the widely variable US and CT presentation of sharp foreign bodies perforating the wall of stomach or bowel.
This pictorial essay is based on a literature search and our personal experience with 49 cases and will enable you to make the correct diagnosis, to understand the natural course and also to help the clinician to choose the best and least invasive treatment.
For critical comments and additional remarks: [email protected]
Introduction
Accidental ingestion of sharp foreign bodies is a potentially life-threatening event.
If a sharp foreign body gets stuck in the pharynx or esophagus, the patient will usually notice its presence and will seek medical help immediately.
If, however, the sharp foreign body, unnoticed by the patient, is able to reach the stomach, it may penetrate at some point, the wall of the stomach, small or large bowel, giving rise to atypical and treacherous symptoms.
This often leads to serious delay and may even be fatal.
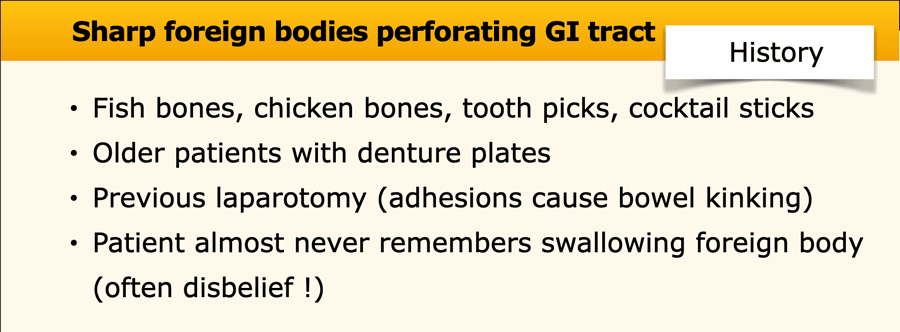
This table contains the key points in the history of the patient.
The ingested foreign bodies are fish or poultry bones and wooden sticks as tooth picks and cocktail sticks.
Patients virtually never remember swallowing, and even show disbelief when confronted with the diagnosis.
The average age is 60 years and many patients wear denture plates.
Patients with perforation of small or large bowel often have a previous laparotomy in their history.
Perforating foreign bodies in stomach and bowel are rarely clinically considered and are increasingly recognized by the use of US and CT, so there is a key role for the radiologist, in primary detection and also in guiding minimal invasive treatment.
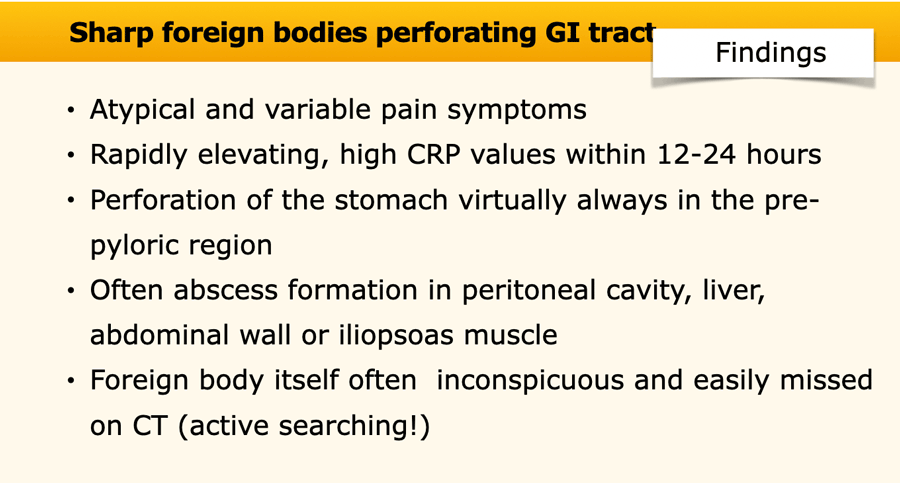
This table contains the key points in the clinical, US and CT findings.
Pain is variable and atypical.
CRP usually rises quickly in the first 24 hours.
Perforation of the stomach always occurs in the prepyloric region.
Abscesses may occur in the peritoneal cavity, abdominal wall, iliopsoas muscle and liver.
The foreign body itself may be rather inconspicuous and is easily missed.
This requires awareness and active searching on CT scan
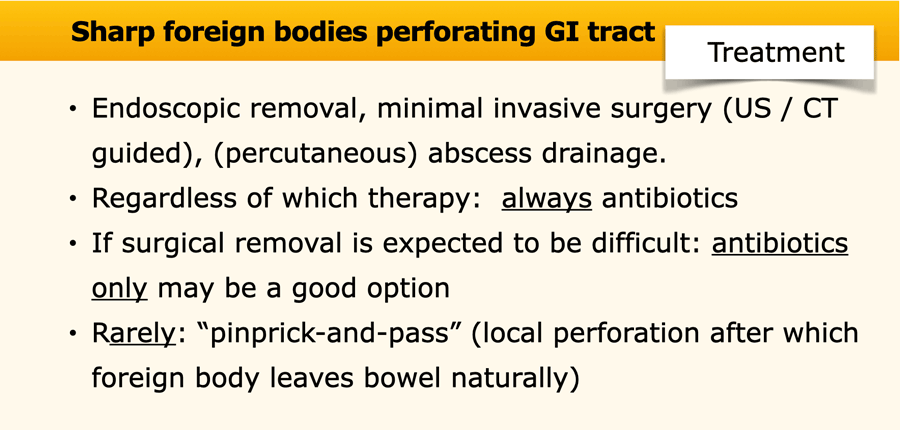
This table contains the key points of the treatment.
Whenever possible, endoscopical removal is the best option, followed by minimal invasive surgery, guided by the US and CT findings.
Abscesses can be drained percutaneously, or evacuated surgically together with removal of the foreign body.
In all instances, antibiotics are mandatory.
Antibiotics alone may be the definitive treatment, especially in case of small fish bones and after successful abscess drainage.
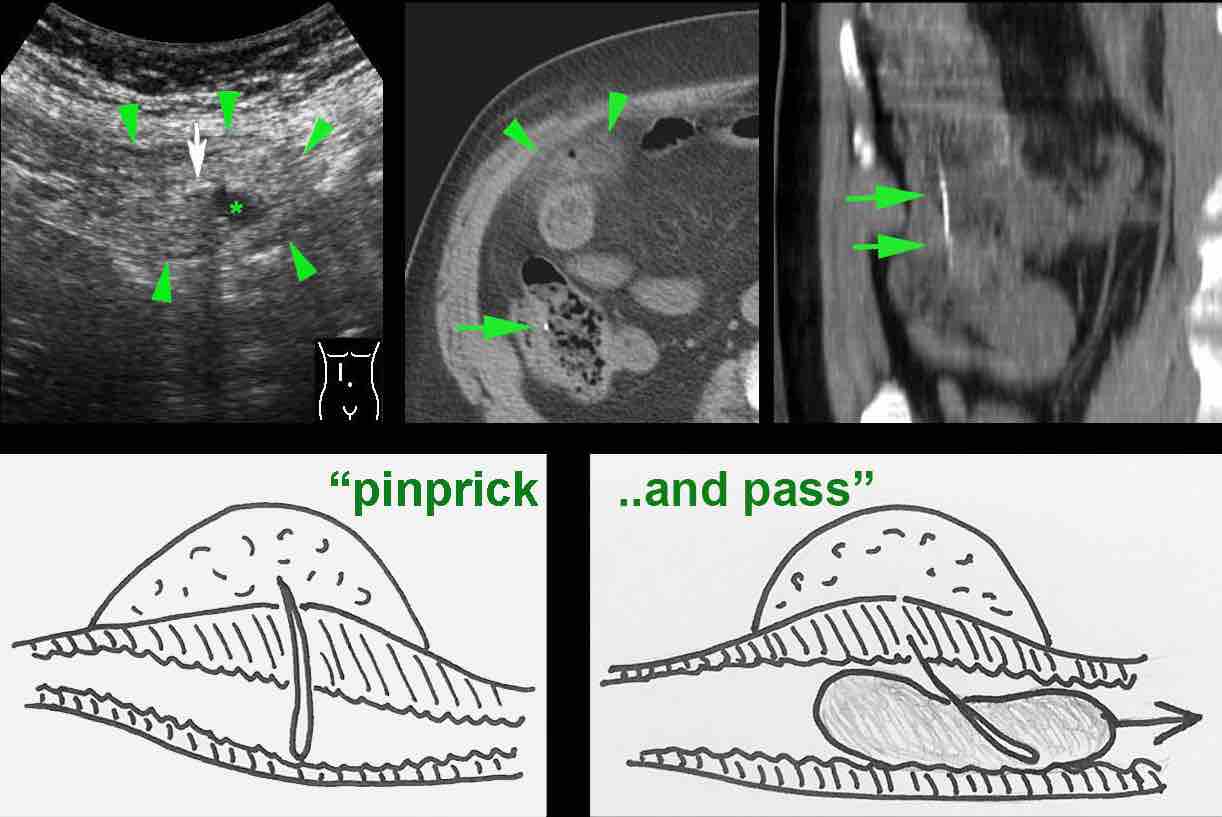
Rarely, the sharp foreign body may cause local perforation and yet leave the bowel naturally.
This is called pinprick-and-pass.
Epidemiology and pathophysiology
It is unknown how often sharp foreign bodies on their journey through the GI tract actually perforate stomach and bowel.
Probably many fishbones eventually pass with the stool without any problem.
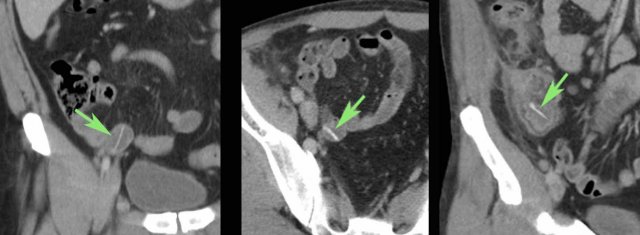
When specifically looked for, it is not uncommon to find hyperdense bones (arrow) in the bowel lumen, as in these three asymptomatic patients.
The most frequently encountered penetrating sharp foreign bodies are fish bones, chicken bones and wooden sticks as toothpicks or cocktail sticks.
The vast majority of patients do not recall having swallowed such an object, and when confronted with the sharp object, often show remarkable disbelief.
Many patients wear denture plates that might render their palatum less sensitive.
It is not always possible to differentiate bones from wooden sticks on CT, but fishbones are generally rather hyperdense and curvilinear, while wooden sticks are less hyperdense and more straight.
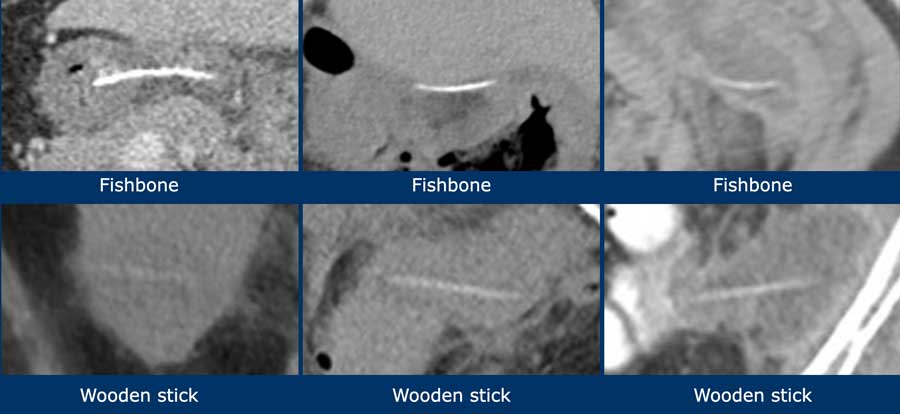
Half of the patients with small bowel perforation, have a history of a previous abdominal surgery.
Adhesions cause local kinking of the bowel loops inhibiting the sharp foreign body to “take the corner”.
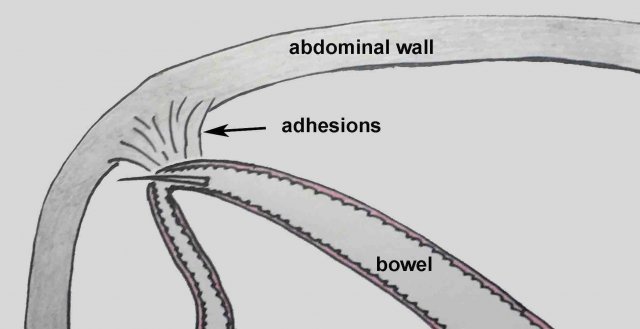
Once a sharp object penetrates the wall of stomach or bowel, omentum and mesentery will try to wall-off the ensuing perforation.
Often, an abscess will develop: in the peritoneal cavity, in the liver, in the abdominal wall or in the iliopsoas muscle.
The foreign body may lie within the abscess, but also remain at its periphery. Sometimes, significant migration of the object may occur.
One third of the perforating sharp foreign bodies lies within reach of either gastroscopy or colonoscopy.
This is obviously the best option for the patient.
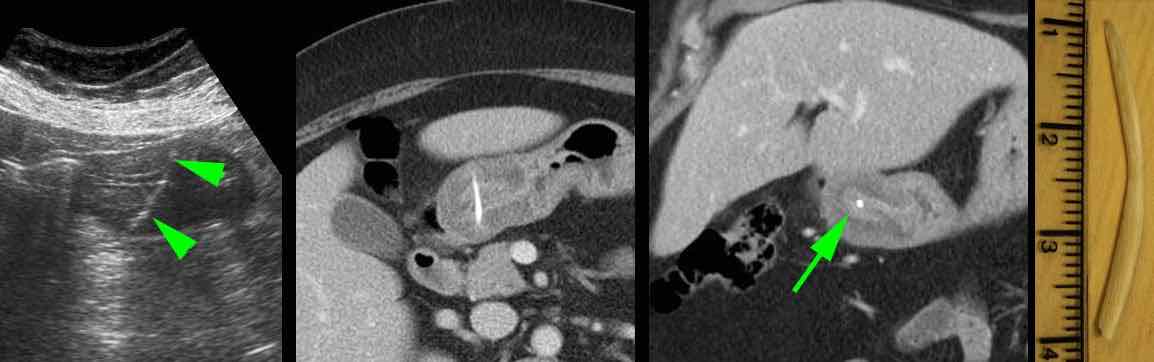
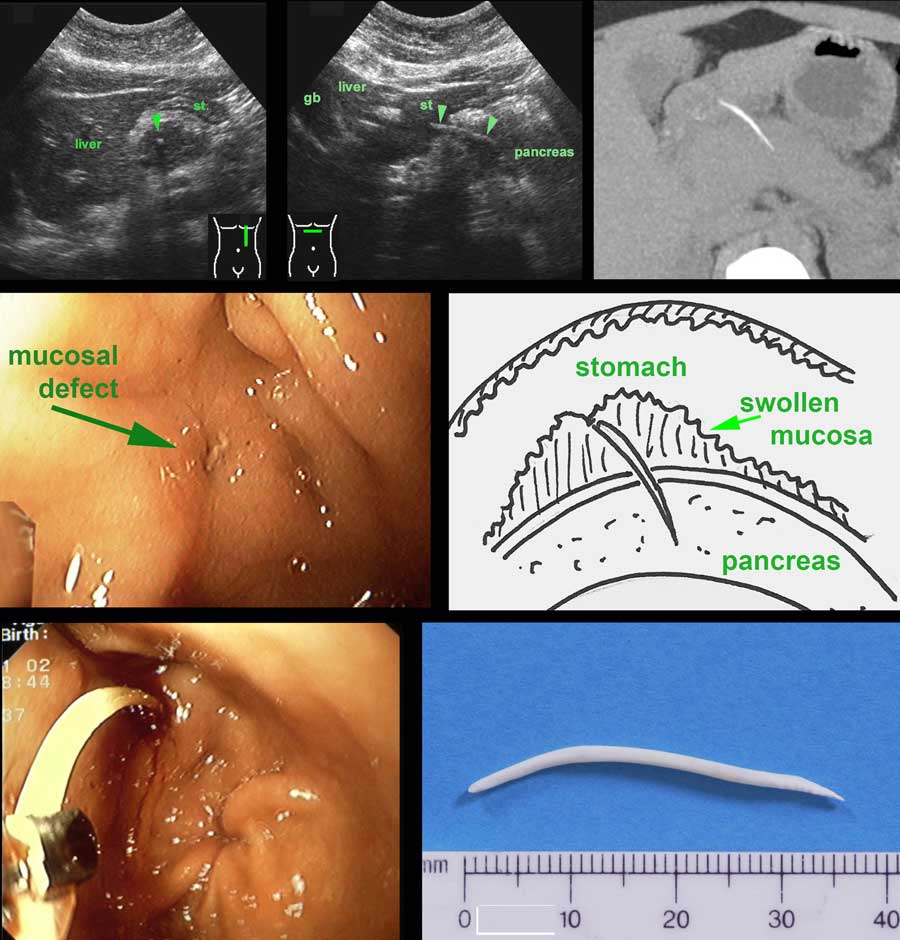
A 59-year old woman with atypical upper epigastric pain for two days.
US reveals remarkable wall thickening of the prepyloric antrum, harbouring a hyperechoic, curvilinear structure (arrowheads), suspect for a fishbone.
CT confirms the diagnosis.
Note how the fishbone (arrow) could easily be missed on the coronal CT alone.
Uneventful recovery after endoscopic removal.
US and CT show a fishbone perforating the stomach wall just before the pylorus.
At gastroscopy no fishbone was found, but only local mucosal swelling with a central ulceration (arrow).
Deep instrumentation with a large forceps into this area eventually succeeded in grabbing the fishbone.
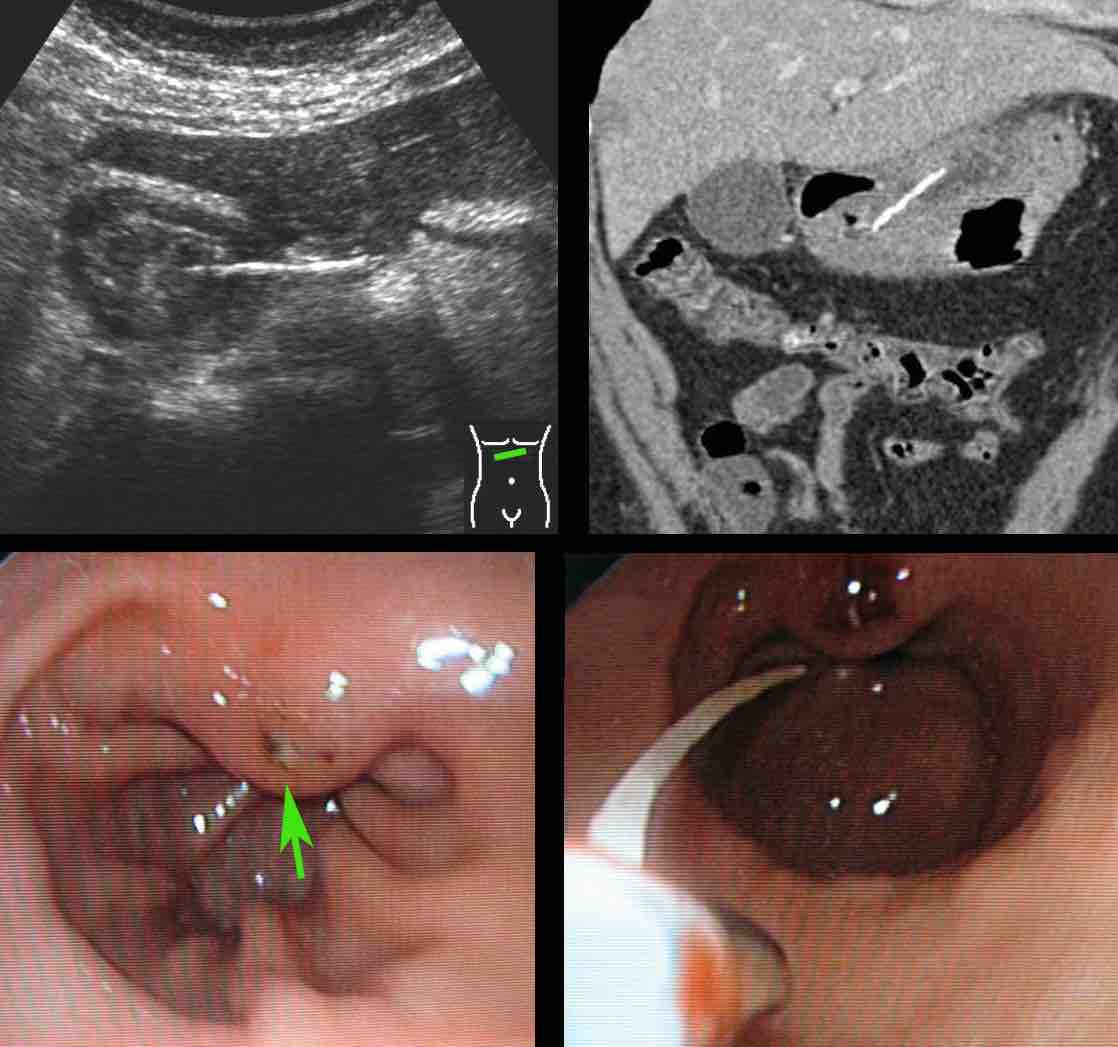
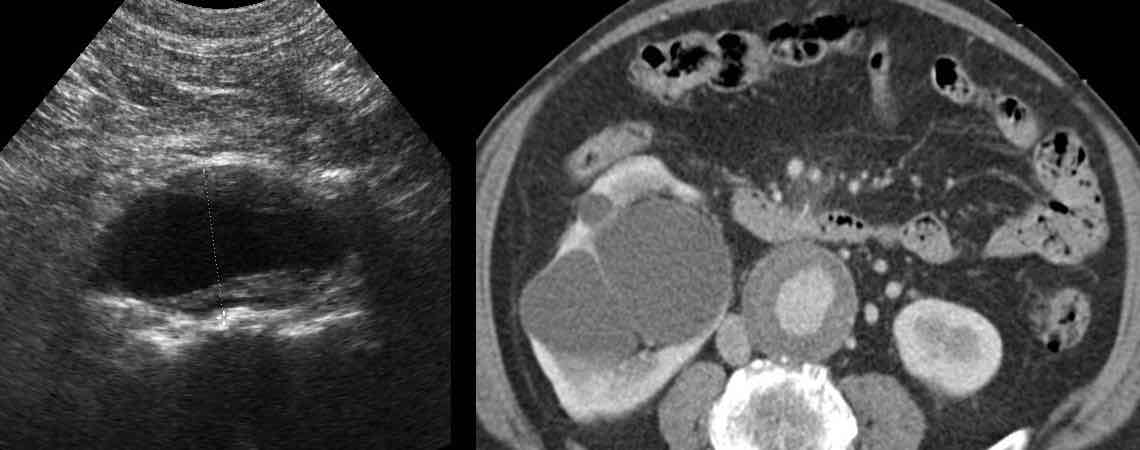
A 74-year old woman presents with deeply located, lower abdominal pain since 3 weeks. Lab: 15 leukocytes, CRP 150. She had multiple gynaecological operations in the past.
CT was done and revealed a bony foreign body, which, at both ends, appeared to perforate the sigmoid.
Endovaginal US confirmed that the foreign body traversed the sigmoid lumen, so colonoscopic removal was possible.
During the endoscopical procedure, the chicken bone had to be broken in two parts in order to be safely removed. Uneventful recovery with help of antibiotics.
If the foreign body is not reachable for the endoscope and is well accessible for the surgeon, in principle surgical removal of the foreign body is indicated.
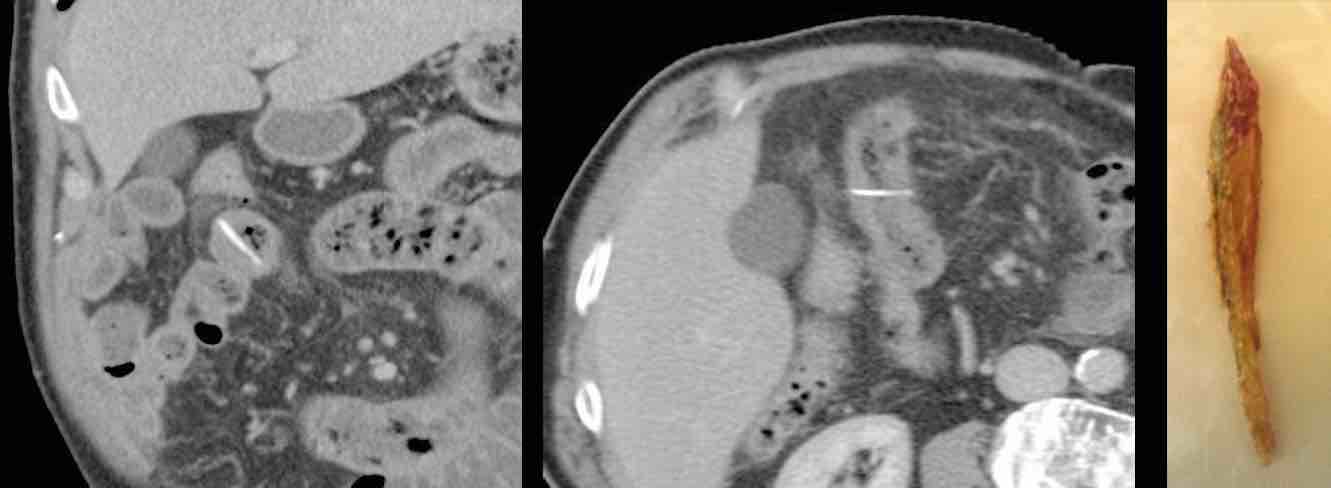
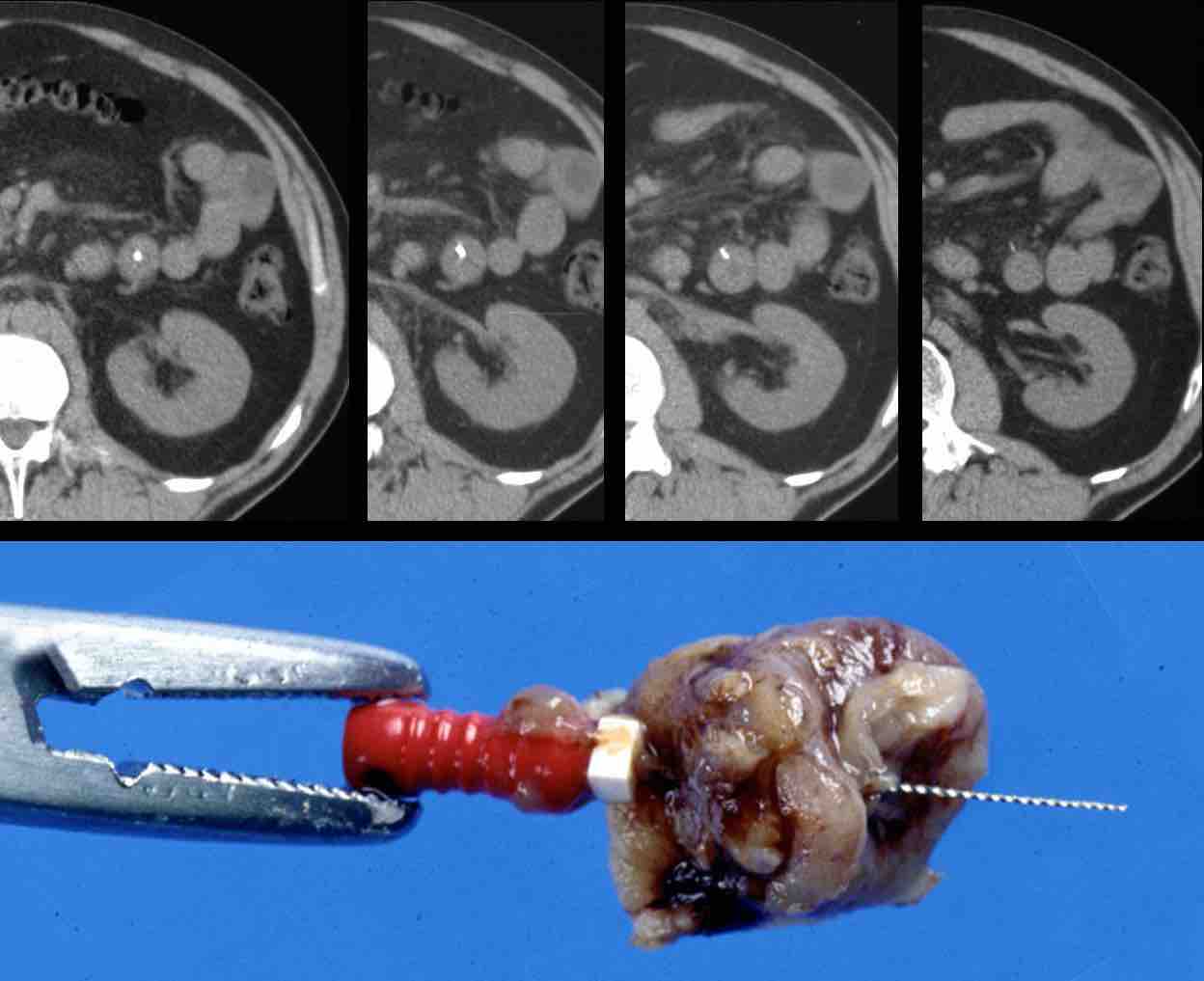
This 33-year old man (with a previous bowel resection at age four) presented with epigastric pain and a CRP of 155. US and CT confirmed a bony structure (arrows) perforating an adhesive small bowel.
At mini-laparotomy a sharp 6 cm bone was removed. The patient ate Peking duck two days earlier.
A vital 83-year old man presented with acute upper abdominal pain and a CRP of 90. CT found a bony structure stuck in the jejunum. After 24 hours of conservative therapy with antibiotics, the pain did not diminish and the CRP went up to 230.
At surgery a sharp, perforating bone chip could easily be removed by means of a small jejunal incision, there was no need for bowel resection.
The patient made a quick recovery and now, eleven years later, at 94, he is still in perfect condition. He can still not imagine that he ever swallowed such a large bone chip
In case of deeply located abscesses as liver abscesses, percutaneous drainage is indicated in combination with long-term antibiotics. In some patients this may be the definitive treatment.
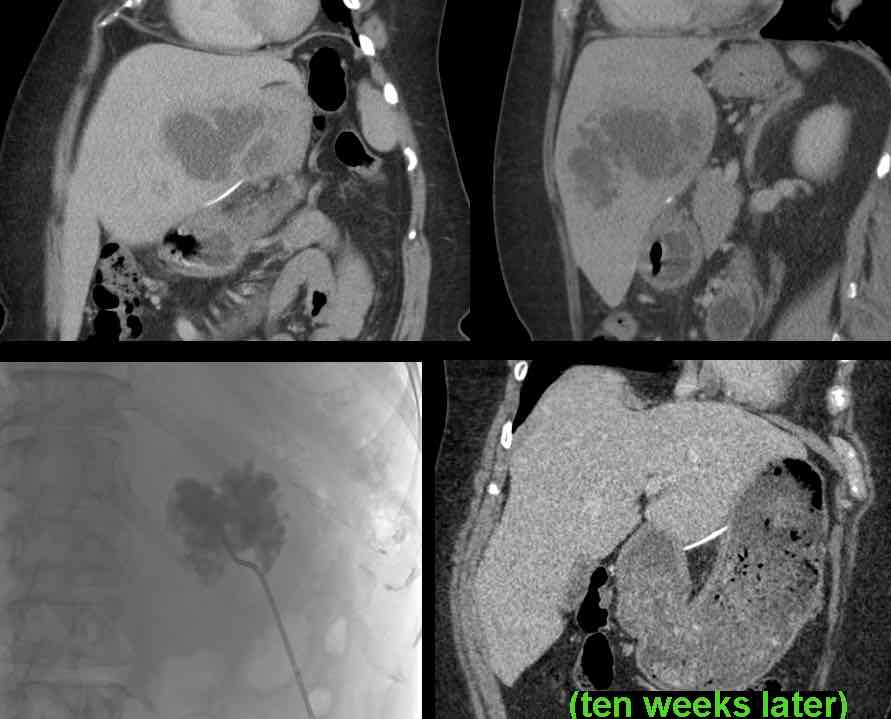
This 61-year old lady presented with a large fishbone-related liver abscess. She was obese and had several other contraindications for surgery.
After multiple percutaneous drainage procedures and ten weeks of antibiotics, she eventually recovered, with the fishbone still in place, apparently encapsulated.
Now, ten years later, she is still doing fine.
At times, it may be very difficult to find the foreign body at laparoscopy or open surgery.
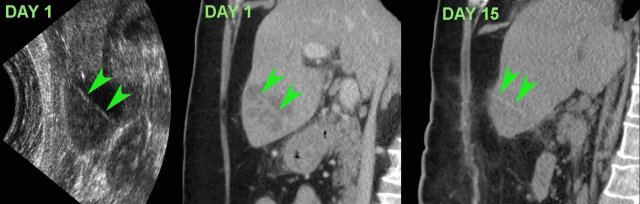
This patient presented with upper abdominal pain and a CRP of 245. US and CT revealed a slightly hyperdense, straight foreign body, probably a cocktail stick (arrowheads) .
At surgery two days later the liver abscess was evacuated, but the foreign body was not found. Afterwards the patient did well on antibiotics.
On day 15, CT showed resolution of the abscess with the foreign body (arrowheads) still in situ. Eventually, the patient recovered with long-term antibiotic treatment.
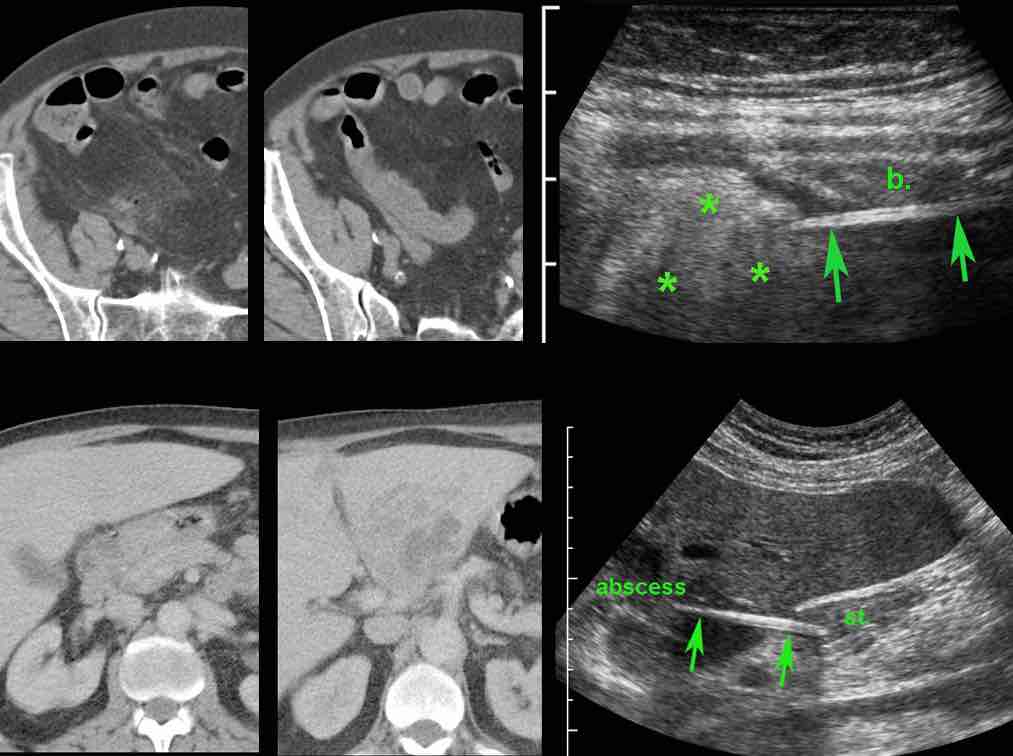
Wooden sticks incidentally may be isodense with the bowel or liver tissue they traverse, and thus may be hardly or not visible on CT scan. In these cases, focused US can be of help.
In patient A, CT findings of an air-bubble, fat stranding and local bowel wall thickening, suggested a local perforation, but no foreign body was seen.
Immediate US of this area unequivocally revealed a sharp foreign body (arrows) piercing through the bowel (b.) wall into the surrounding inflamed fat (*).
In patient B, antral wall thickening and a nearby liver abscess, suggested a perforating foreign body, which however could not be identified on CT.
US, performed with knowledge of the CT findings, easily detected the, apparently isodense, foreign body. (st. = stomach)
Often no abscess occurs and the fishbone, after migration, becomes encapsulated. Antibiotics may be of help in the encapsulation process.
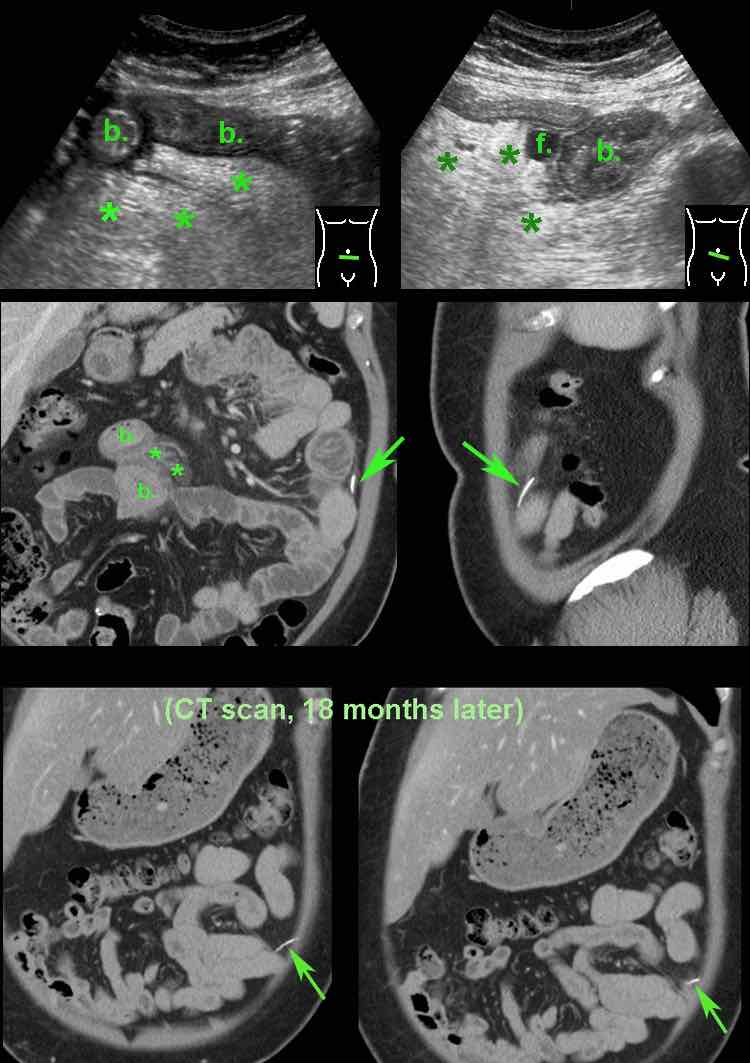
This 48 year old woman was submitted with severe periumbilical pain since 12 hours (Lab: 15 leukocytes, CRP 7).
The next day the pain subsided, but the CRP went up to 65.
US of the periumbilical area, showed edematous wall thickening of small bowel (b.) with normal peristalsis.
There was a tiny fluid collection (f.) and inflammation of the hyperechoic and non-compressible mesentery (*).
Subsequent CT confirmed small bowel wall thickening (b.) and fat stranding (*) in the mesentery. In the left paracolic gutter, a fishbone (arrow) was found.
Apparently the fishbone, after perforating the jejunum, did migrate to that spot.
Subsequent laparoscopical exploration was unable to identify the fishbone.
She made an uneventful recovery with antibiotics.
CT scan, performed for other reasons 18 months later, showed slight migration of the fish bone, apparently well-encapsulated.
Patient is still doing well eight years later.
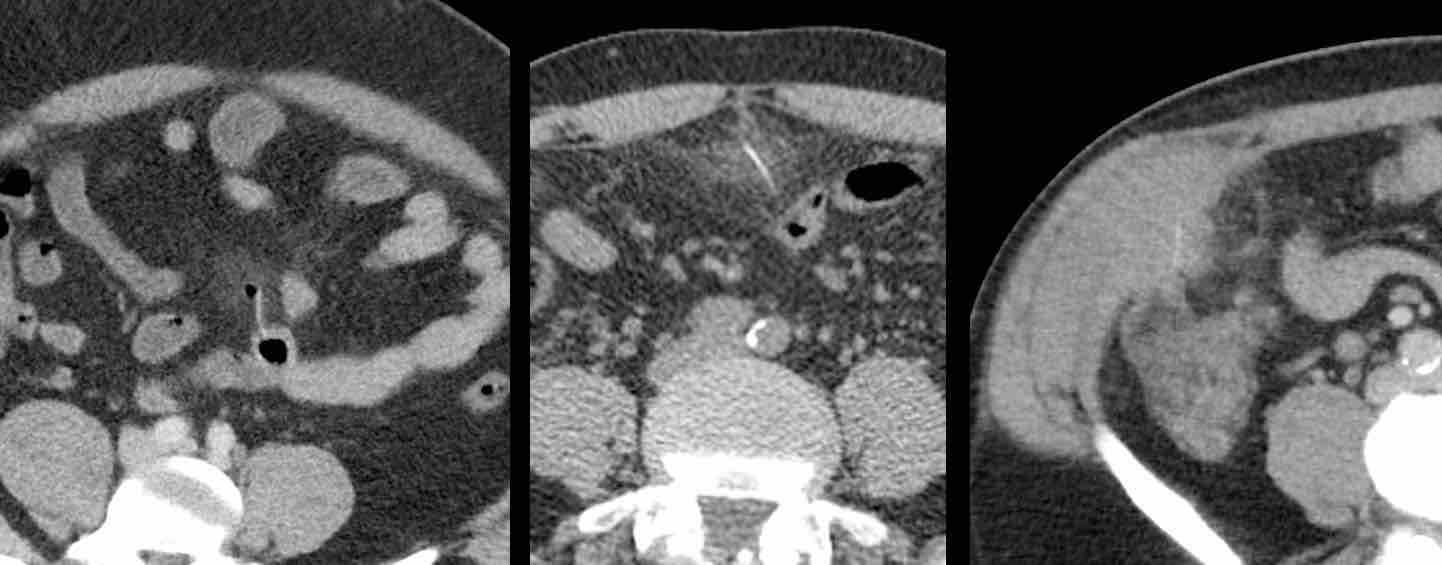
In case of relatively mild symptoms in patients with small, perforating fishbones without an abscess, primary antibiotic treatment may be a good first option.
These three different patients all made an uneventful recovery with antibiotics only.
Sometimes nature is very mild.
This 72 year old lady presented with acute epigastric pain and a CRP of 180, caused by a fishbone, perforating her stomach.
Only proton pump inhibitors were given.
Her symptoms rapidly subsided and her CRP was normal again in three days.
She made a full recovery, and 11 years later is still doing fine.
Two different patients with an encapsulated fishbone in the wall of the antrum as coincidental finding on CT, performed for other reasons.
Both patients did not recall a period of upper epigastric pain and had unchanged CT images for many years.
In case of an abdominal wall abscess, surgery can be done in order to drain the abscess and remove the foreign body.
In this patient, only a small peri-umbilical incision allowed evacuation of pus and removal of the fishbone.
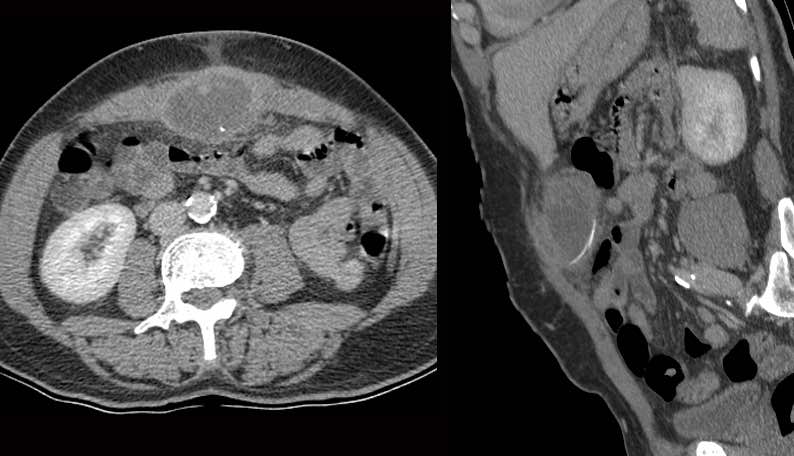
This 58-year old patient presented with pain LLQ and a CRP of 105, suspect for diverticulitis.
US found a ovoid mass of inflamed fat (arrowheads) lateral of the sigmoid, suggestive of epiploic appendagitis.
Subsequent CT revealed a straight, hyperdense foreign body (arrows) surrounded by fat stranding.
The patient was treated with antibiotics.
One week later an abscess did develop, which was percutaneously drained.
Eight weeks later a cocktail stick was removed as an elective procedure.
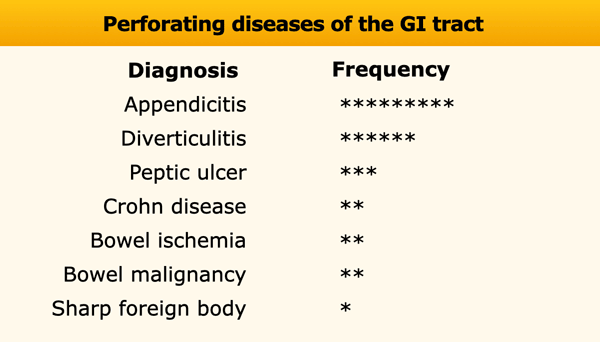
Perforating diseases of the GI tract
Causes of perforation
If at US or CT bowel wall thickening is found in combination with fat stranding, free air configurations and/or abscess formation, it is not always clear what the underlying cause is.
The mnemonic PSI-ABCD may be helpful:
- Peptic ulcer
- Sharp foreign body
- Ischemic bowel
- Appendicitis
- Bowel carcinoma
- Crohn's disease
- Diverticulitis
In the table, the star-classification indicate the frequency of these potentially perforating conditions.
In 99,99 % of cases, one of these seven conditions is the cause of the perforation or walled-off perforation.
In our hospital we have a relatively large number of sharp, perforating foreign bodies of 3-4 cases per year.
This is partially explained by a large immigrant population, eating exotic fish species.
Especially Surinamese people who make up 30 % of our patients, are responsible for 70% of the fishbone perforations.
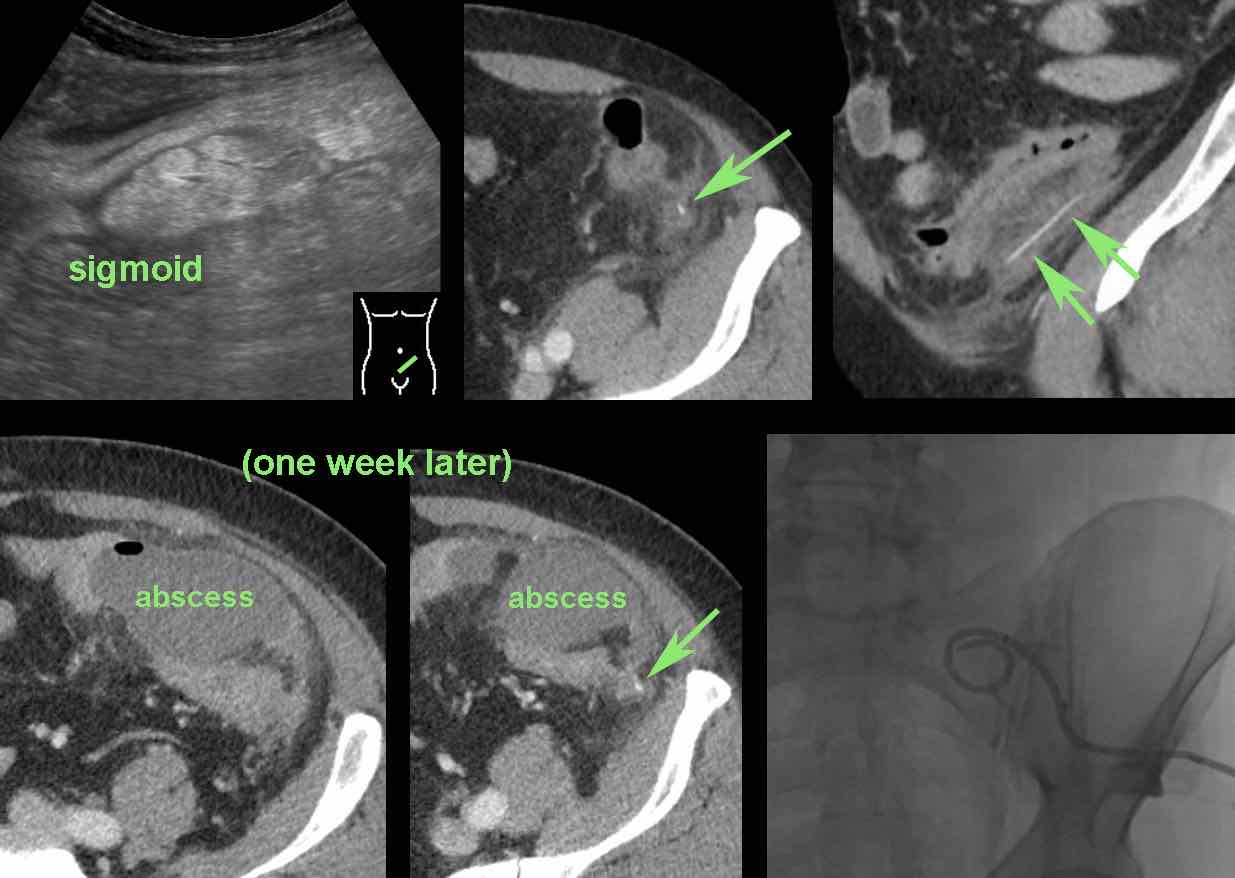
Pinprick-and-pass
A sharp foreign body may cause a perforation, but may yet pass normally with the stool (”pinprick-and-pass”).
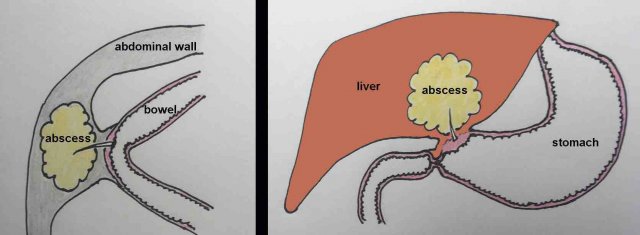
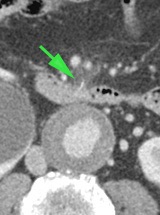
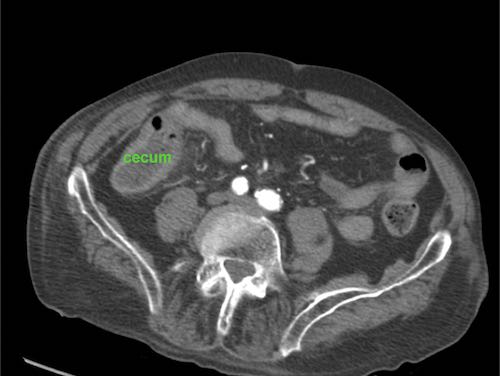
This 85-year old man presented with severe localized pain, focal peritonitis and a CRP of 200, clinically suspect for appendicitis.
US showed a small focal area of inflamed hyperechoic fat (arrowheads), harbouring a little fluid (*) and an ill-understood reflection (white arrow).
The presumed US diagnosis was epiploic appendagitis with a small central area of hemorrhage.
CT confirmed local fat stranding and detected an air bubble as well as slight wall thickening of a neighbouring small bowel loop.
Using the mnemonic PSI-ABCD, all conditions were excluded, except for a sharp foreign body.
After specific searching a fishbone was detected in the cecum (green arrows on CT).
Apparently, this fishbone had caused a perforation, and was later propelled by some small bowel contents. The patient was treated with antibiotics only and made a full recovery.
Illustrative cases
This 37-year old woman had progressive epigastric pain since 4 days.
US detected a reflective curvilinear structure (arrowheads) reaching from the stomach (st.) into the swollen pancreas, suspect for a fishbone. (gb=gallbladder).
CT without contrast confirmed a fishbone stuck in the pancreas.
At gastroscopy, no fishbone was seen, only a small mucosal defect producing some fibrin strands.
We assumed that this was the point where the fishbone must have penetrated while the remaining end of the fishbone got “buried” in the reactively swollen mucosa of the posterior stomach wall (see drawing).
Encouraged by this knowledge the endoscopist performed deep instrumentation with a large forceps, which eventually was successful.
The patient made a full recovery and told us having eaten “jarabaka” a week earlier, a Surinamese fish, known for its delicious taste and its sharp bones.
A 81-year old man with progressive epigastric pain for 24 hours.
US revealed an aortic aneurysm of 5.2 cm.
Immediate CT scan excluded rupture, however some subtle fat stranding anterior of the duodenum was seen around a small hyperdense structure.
CT revealed a fishbone (arrow) in the duodenum, perforating its ventral wall.
At gastroscopy the fishbone was easily recognized and removed.
Note the greenish discoloration of the fishbone due to bile pigments.
When confronted with the results, the patient could not imagine ever having swallowed such a large fishbone.
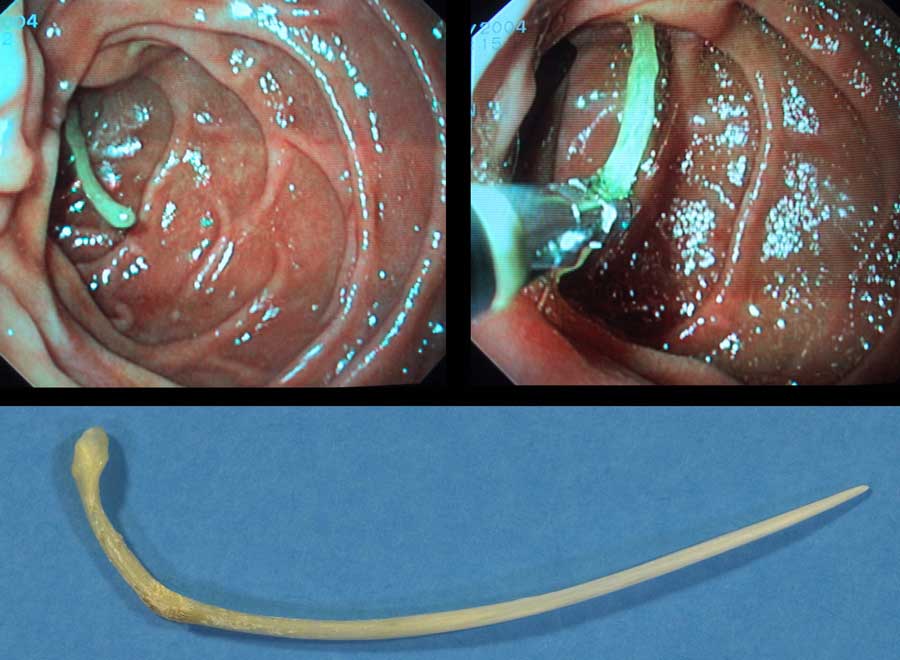
A 50 year old man with pain LLQ and a CRP of 21, suspect for diverticulitis.
Initial US shows wall thickening of the sigmoid, inflamed fat (*) and a fecolith within a diverticulum (white arrowhead).
Closer inspection of the area where the most inflamed, non-compressible fat (green arrowheads and *) was seen, revealed a foreign body (arrows).
CT without contrast confirmed a piece of bone and subtle fat stranding (*) around the sigmoid.
Endoscopic removal was relatively easy.
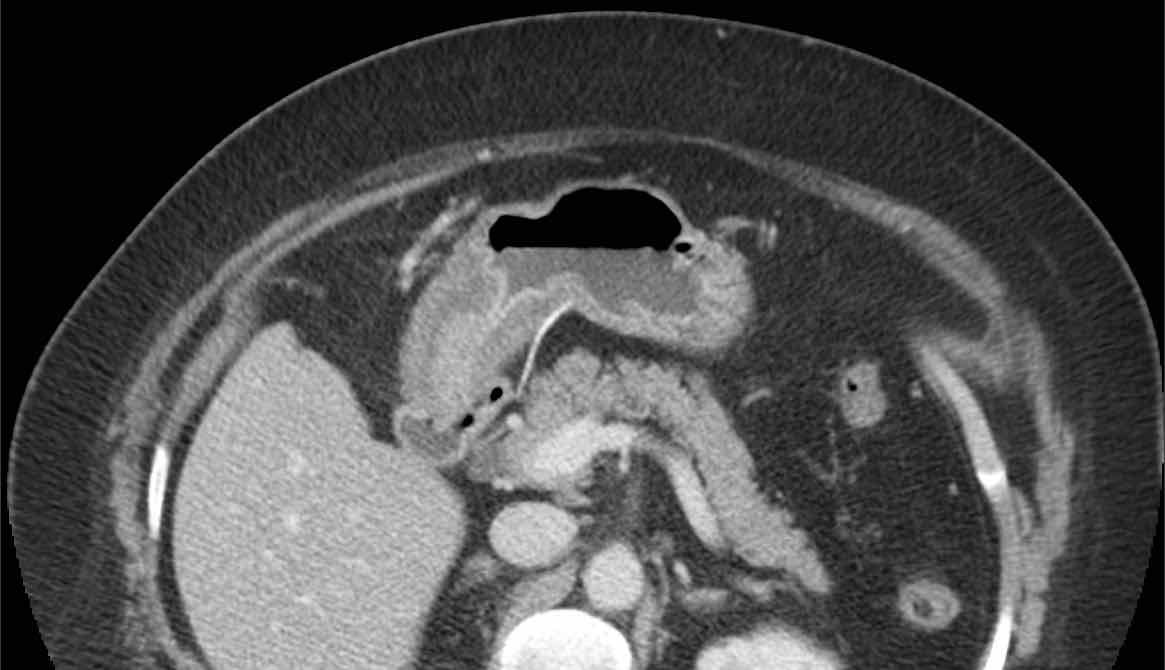
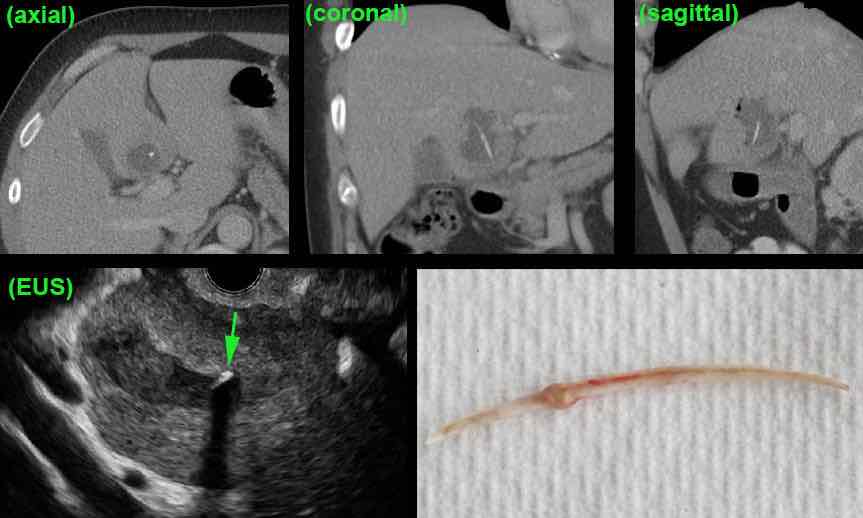
This is a 60-year old woman with high fever and clinically possible pancreatitis.
CT scan showed an abscess in the quadrate lobe, harbouring a fishbone, migrated from the stomach to the liver.
Endoscopic US confirmed the fishbone entirely within the liver abscess (arrow), so endoscopic removal was impossible.
At surgery, the abscess was drained and the fishbone removed.
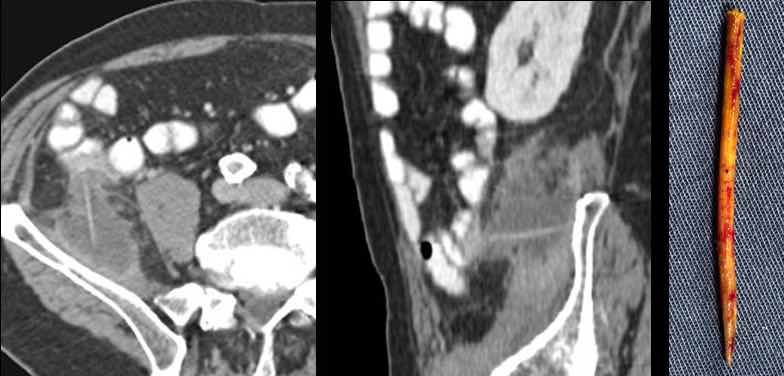
A 75 year old man with a clinically suspected iliopsoas abscess.
CT confirms the abscess and identified a straight, slightly hyperdense sharp foreign body, apparently migrated from the small bowel to the iliac muscle.
Shape and density suggested a wooden pen rather than a fishbone.
With only minimal invasive surgery, both pus and wooden pen were removed.
Patient had artificial denture, a previous appendectomy and had the habit of “shoving-off” meat of his sateh-pen with a fork.
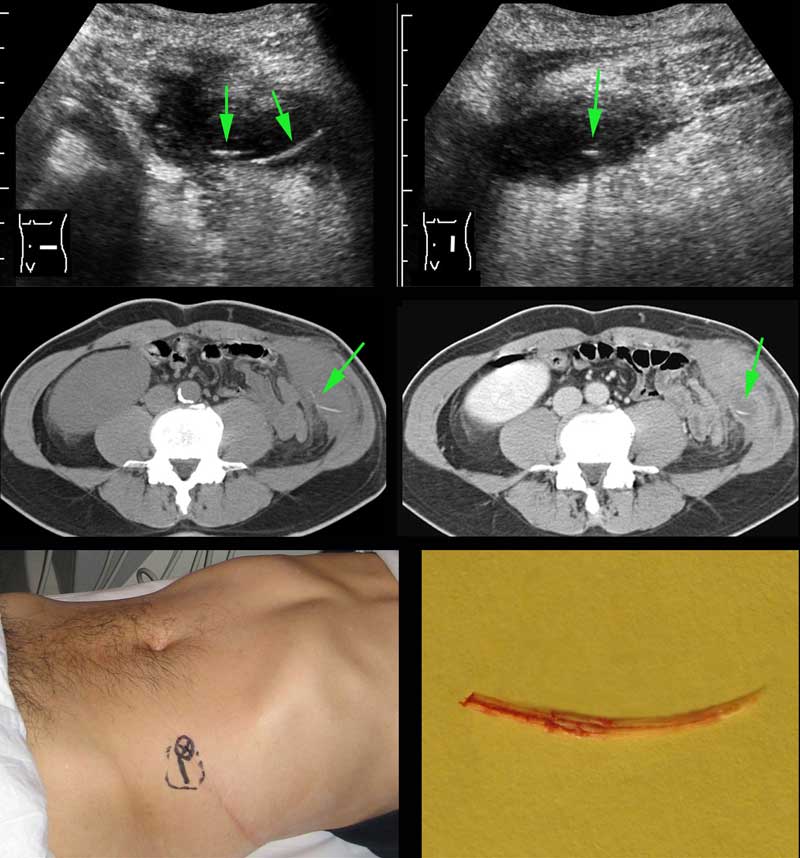
A 53-year old man presented with a painful LLQ swelling and a CRP of 173, suspect for diverticulitis.
He had a left nefrectomy 20 years ago.
US revealed an abscess in the abdominal wall harbouring a thin, curvilinear structure (arrow).
CT without and with i.v. contrast, confirms a fishbone (arrow) within a moderately defined, abdominal wall abscess.
Note how easily the fishbone could have been missed if only i.v. contrast CT had been made.
Location of abscess and fishbone were indicated on the skin.
Using only a very small incision, pus and fishbone could be removed. Uneventful recovery.
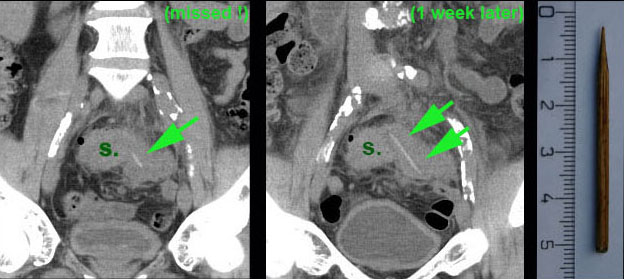
A 57-year old man (previous appendectomy) with suspected diverticulitis.
CT showed thickening of the sigmoid (s.) wall and an unclear mass at the left side.
At this time, the small hyperechoic line (arrow) was missed.
The CT diagnosis was sigmoid diverticulitis or sigmoid malignancy.
Colonoscopy was unable to reach the area.
On a repeated CT one week later, we were lucky that the straight and slightly hyperechoic sharp foreign body (arrows) now presented in its full length on the coronal CT.
At surgery, part of the sigmoid was resected together with a large inflammatory mass, harbouring the causative wooden cocktail stick.
A temporary stoma was made.
The patient showed disbelief and firmly denied ever having swallowed such a stick.
During an endodontal procedure by his dentist, this 46 year old man accidently swallowed an “endofile”.
He had no abdominal complaints, but became worried when, after a week, he did not find it in his stool.
CT without contrast confirmed perforation of a jejunal loop, with only minimal fat stranding.
At surgery a part of the jejunum was resected including the endofile.
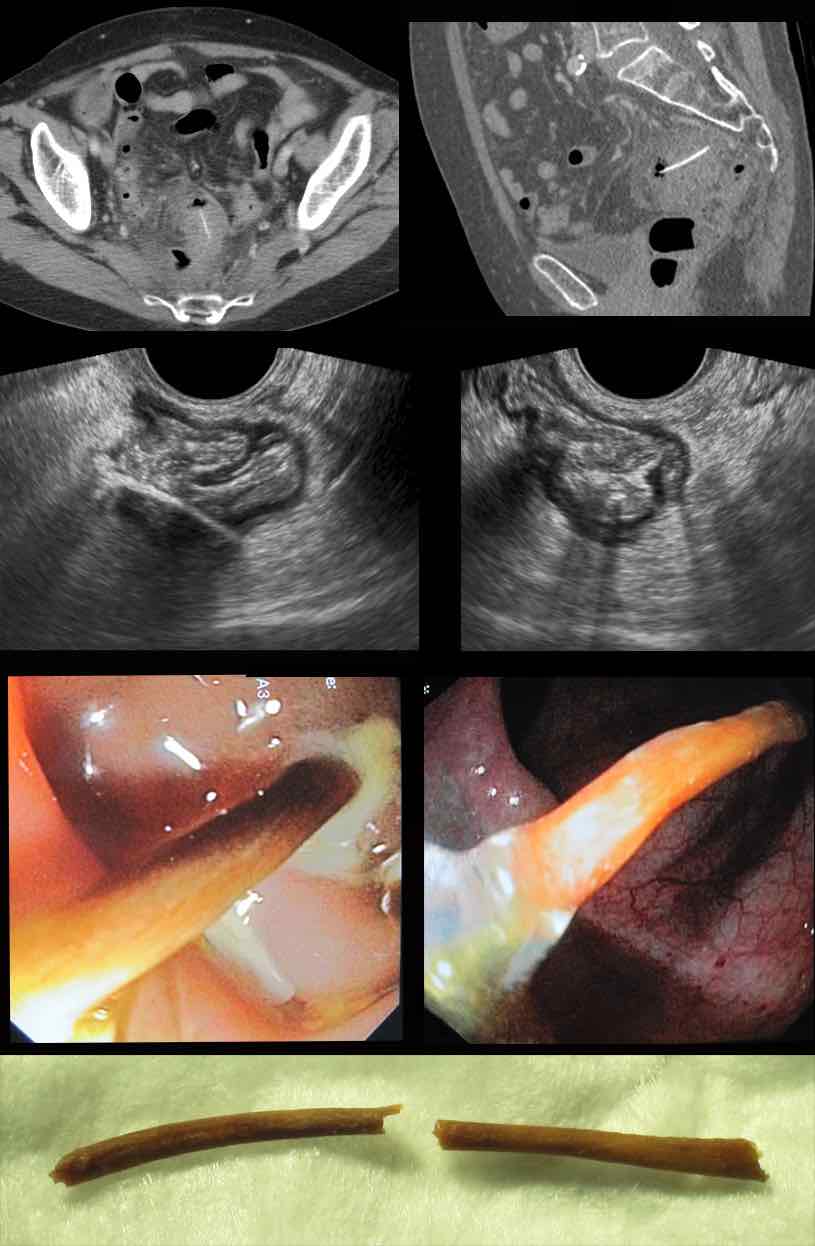
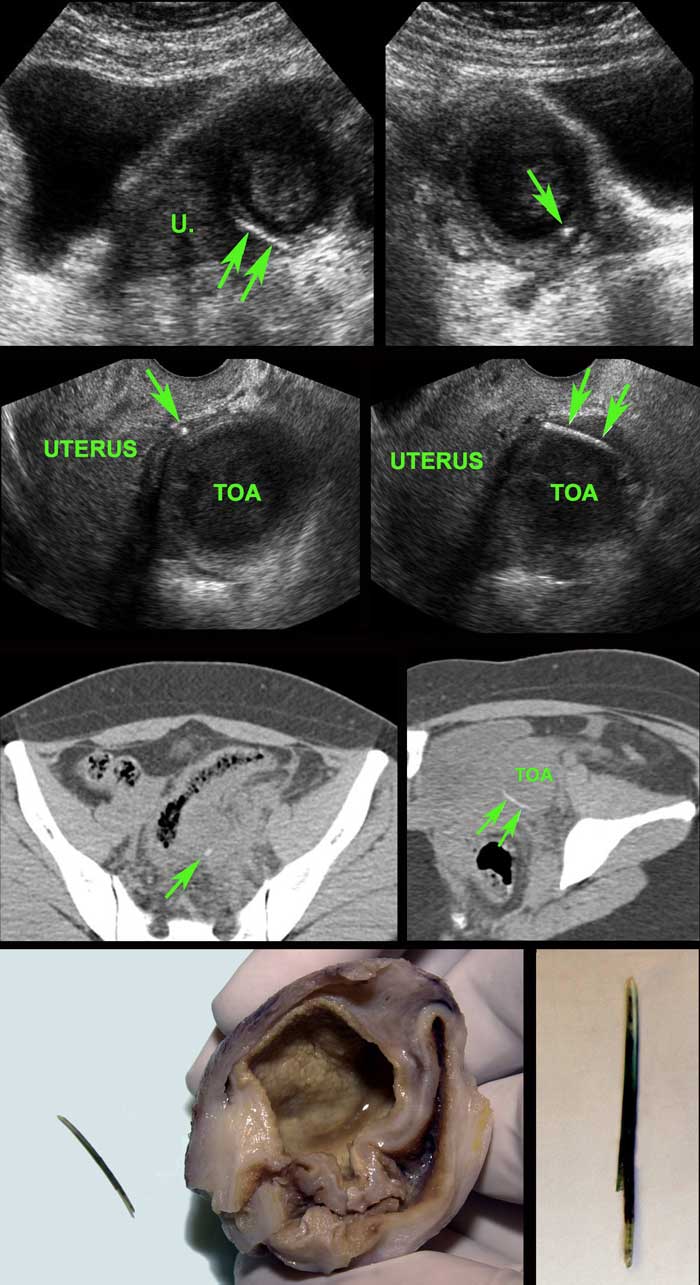
Young (31 years) Surinamese woman with 3 weeks of pain LLQ and CRP 55, suspect for adnexitis or diverticulitis.
Previous history of uterine rupture.
US shows hypoechoic mass left of the uterus (u.) suspect for tubo-ovarian abscess (TOA).
In the periphery a thin, curvilinear reflection (arrows) is seen.
Endovaginal US confirms a fishbone (arrows) in the wall of the TOA.
Non-contrast CT reveals that the TOA has a close relation to the sigmoid, which also shows focal wall thickening.
At surgery, TOA and fishbone, densely adhered to the sigmoid, were removed.
Apparently, the fishbone, after perforating the sigmoid, migrated into the left ovary, causing a TOA.
Note the greenish discoloration of the fishbone, probably due to biliary pigments.
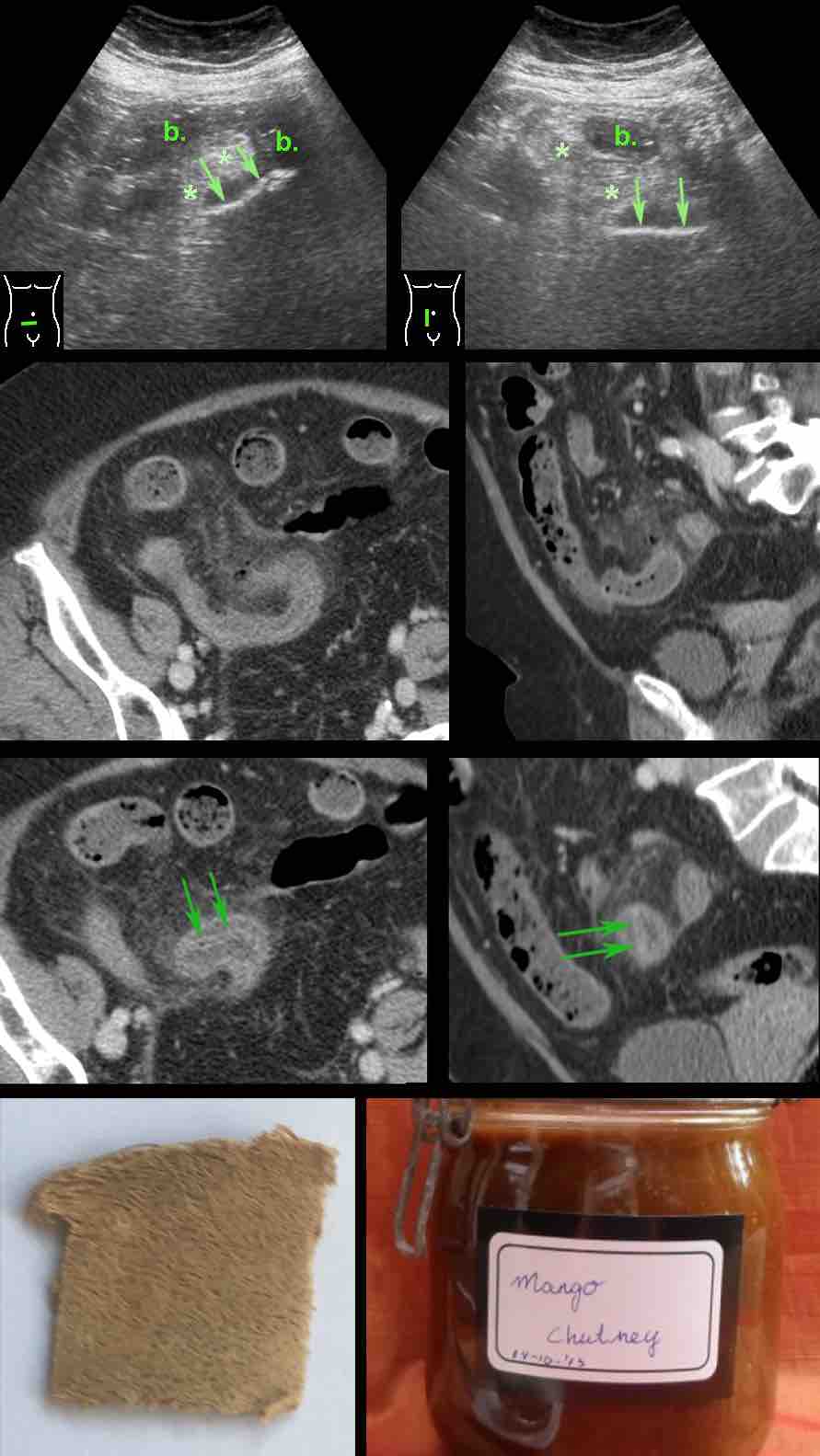
Obese 80 year old lady with strong clinical suspicion of appendicitis.
She had a previous cholecystectomy.
Lab: leukocytes 21, CRP 125.
US showed inflamed fat (*) around edematous small bowel (b.), containing a strange reflective structure (arrows).
The US images in two perpendicular planes, suggested that this foreign body had a flat nature.
CT confirmed small bowel wall thickening, fat stranding and extra-luminal air.
Closer inspection in the axial and coronal CT plane, revealed an intraluminally localized, slightly hyperdense, double-layered flat structure (arrows) of unknown origin.
Surgery revealed focal small bowel usuration by a sharp vegetable peel.
After the operation, this was recognized by the patient as the peel of an unripe mango, used in her self-made mango chutney.
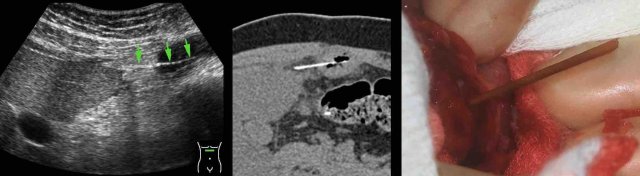
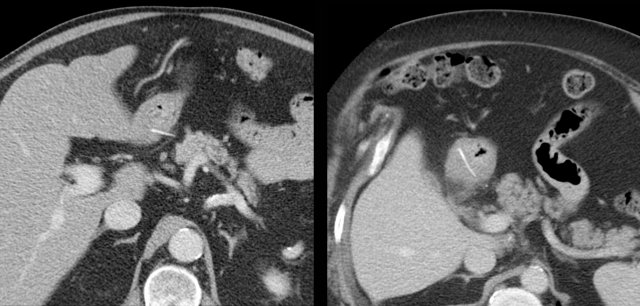
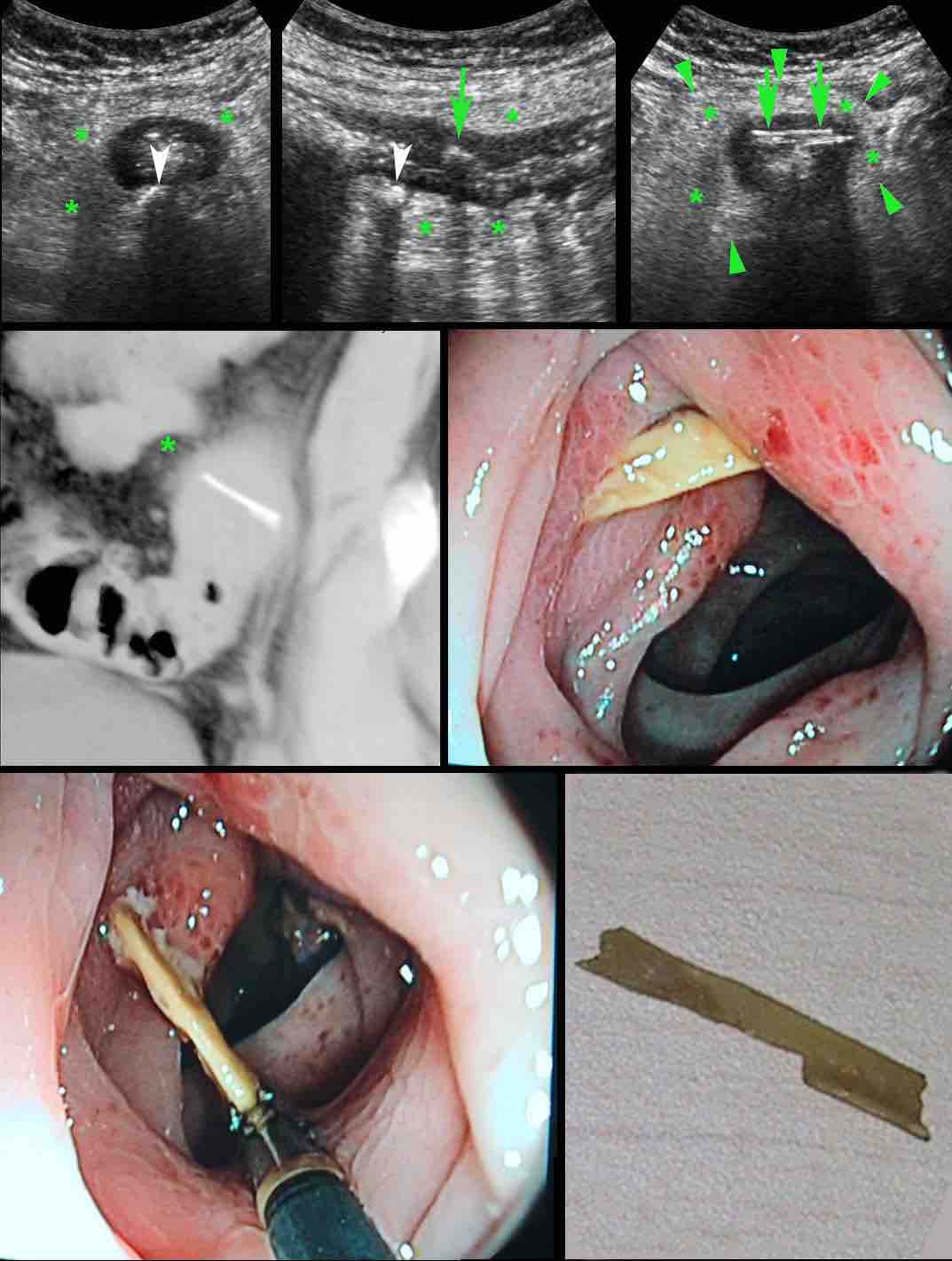
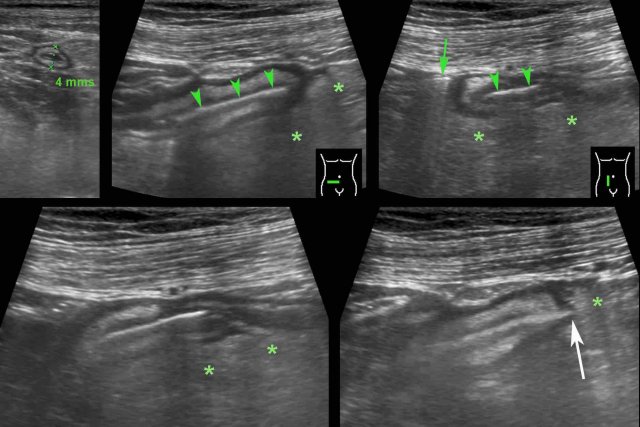
Man of 79 years old, two days hospitalized for myocardial infarction, suddenly developed pain in the RLQ and a CRP of 70, suspect for appendicitis.
He was nursed in isolation for suspected MRSA.
US showed a normal appendix of 4 mms and wall thickening of the terminal ileum, surrounded by inflamed fat (*).
Next to the ileum a possible air bubble (green arrow) was observed.
Within the ileal lumen, a linear reflective structure (arrowheads) was found.
The aspect in multiple planes, suggested a flat foreign body.
On one end, a apparently sharp edge (white arrow) stuck out into the surrounding inflamed fat (*).
Axial CT confirmed the US findings and identified an odd-looking foreign body.

On coronal CT the odd-looking foreign body had the same shape.
Try to figure out, what it is ...
And then continue reading