Cystic Lung Disease - Differential diagnosis
Joline Trap-de Jong¹, Robin Smithuis² and Marcela Spee-Dropková³
¹St Antonius hospital in Nieuwegein ²Alrijne hospital in Leiden and ³Groene Hart hospital Gouda in the Netherlands
Publicationdate
In this article we describe an algoritm to establish a differential diagnosis in cystic lung disease.
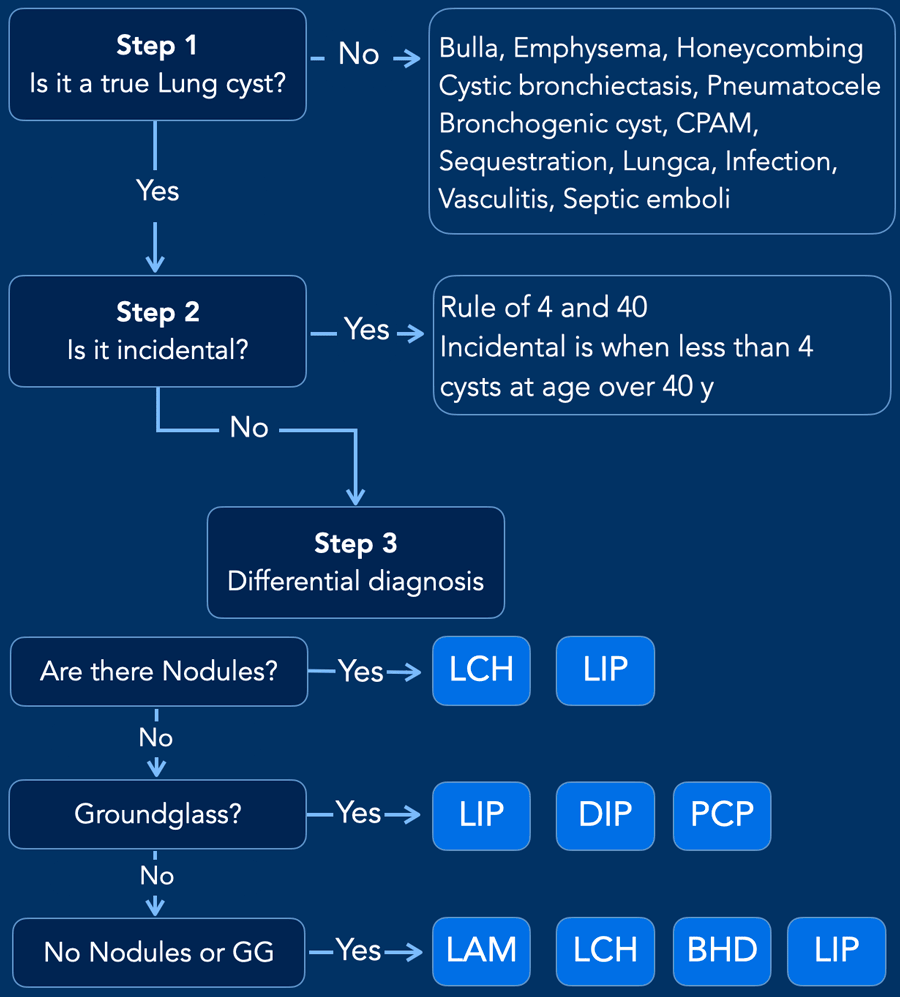
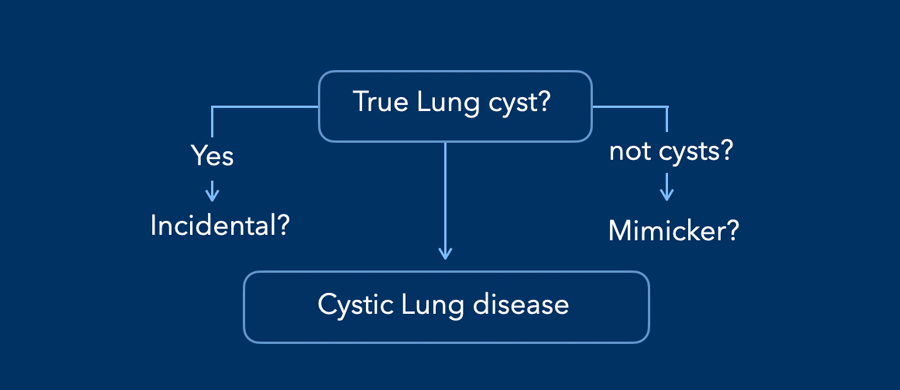
When you encounter something in the lung that looks like a lung cyst, you should ask yourself the following three questions:
- Is it truly a lung cyst or something else?
- Is it just an incidental finding without any clinical significance or should we consider a cystic lung disease?
- How do we establish a differential diagnosis when we think of a cystic lung disease?
Diagnostic Approach
Step 1 - Is it a lungcyst or a cyst-like lesion
A lung cyst is a lucency with a thin (<2mm) regular wall.
In the next paragraph we will discuss how cysts can be differentiated from cavities, emphysema, pneumatocele etc.
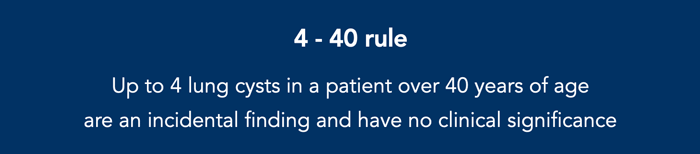
Step 2 - Is it an incidental finding or should we worry
Lungcysts are regarded as incidental finding without any clinical significance if there are less than four cysts in individuals older than forty.
This is called the rule of 4 and 40.
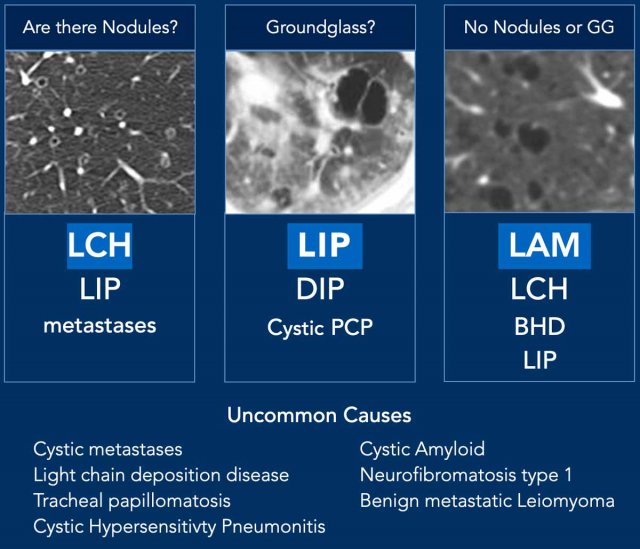
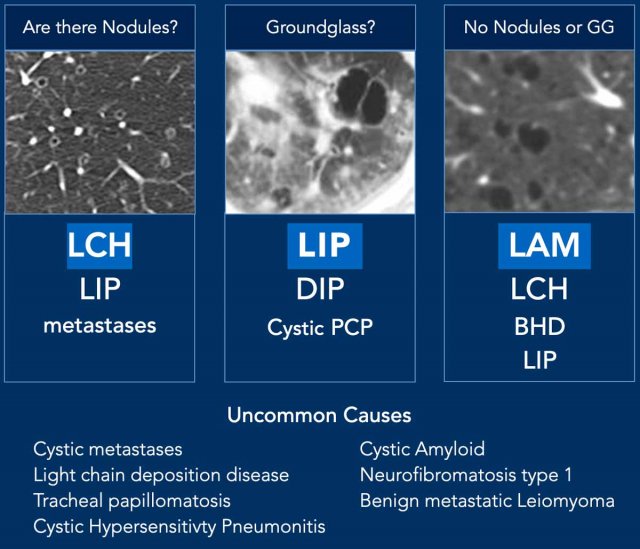
Step 3 - You are probably dealing with a cystic lung disease
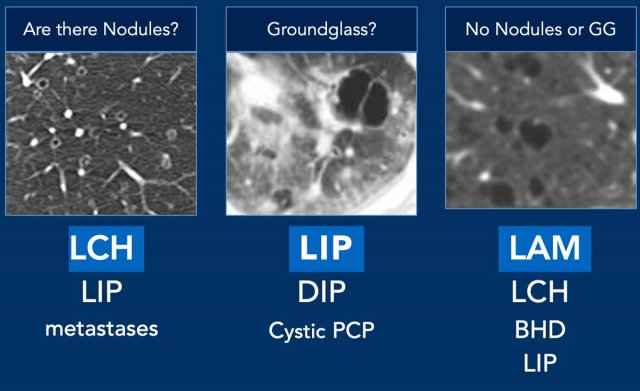
Are there also Nodules - Think LCH and LIP.
Any Ground Glass - Think LIP, DIP and PCP
No Nodules or Groun Glass - Think BHD, LAM, LCH and LIP.
LCH - Langerhans Cell Histiocytosis is a multi-organ disease with a strong association to smoking. There are nodules, cavitating nodules and bizarre cysts that spare the sinus pleurae.
LIP - Lymphocytic Interstitial Pneumonia is associated to Sjogren and HIV. Cysts sometimes with ground glass or small nodules. Limited number of cysts predominantly in lower lung fields and sometimes diffuse.
DIP - Smoking. Basal, peripheral and symmetric cysts within area of ground-glass. Often also fibrosis.
PCP - Infection in immuno-compromised. Ground-glass is dominant. Cysts appear later or when profylactic medication.
BHD - Birt-Hogg-Dubé syndrome is a hereditary condition associated with skin tumors, increased risk of RCC and a limited number of cysts predominantly peripheral in lower lung fields.
LAM - Lymphangioleiomyomatosis. Women, common, spontaneous pneumothorax, pleural effusion. Many, diffuse, round and small cysts. Association with renal angiomyolipomas and Transitional Cell Carcinoma
Step 1: Is it a lungcyst or a cyst-like lesion
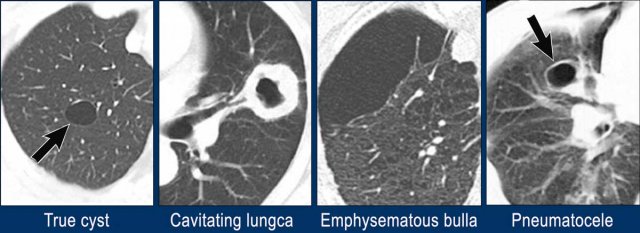
Solitary lesion
A simple lung cyst has a fine thin surrounding wall.
In the figure some solitary lesions that may simulate a lung cyst.
- Simple lung cyst with a smooth thin wall
- Cavitation with a thick irregular wall as can be seen in malignancy or infection like TB.
- Emphysematous bulla without a wall in a patient with centrilobular emphysema
- Pneumatocele. This can look like a simple cyst, but usually there is a history of a chest trauma or ventilation with barotrauma or sometimes as a result of infection.
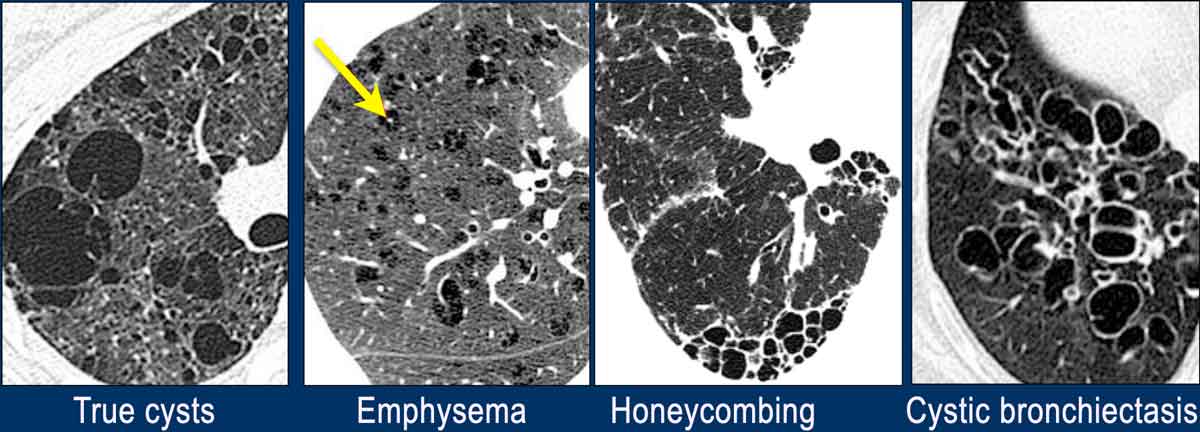
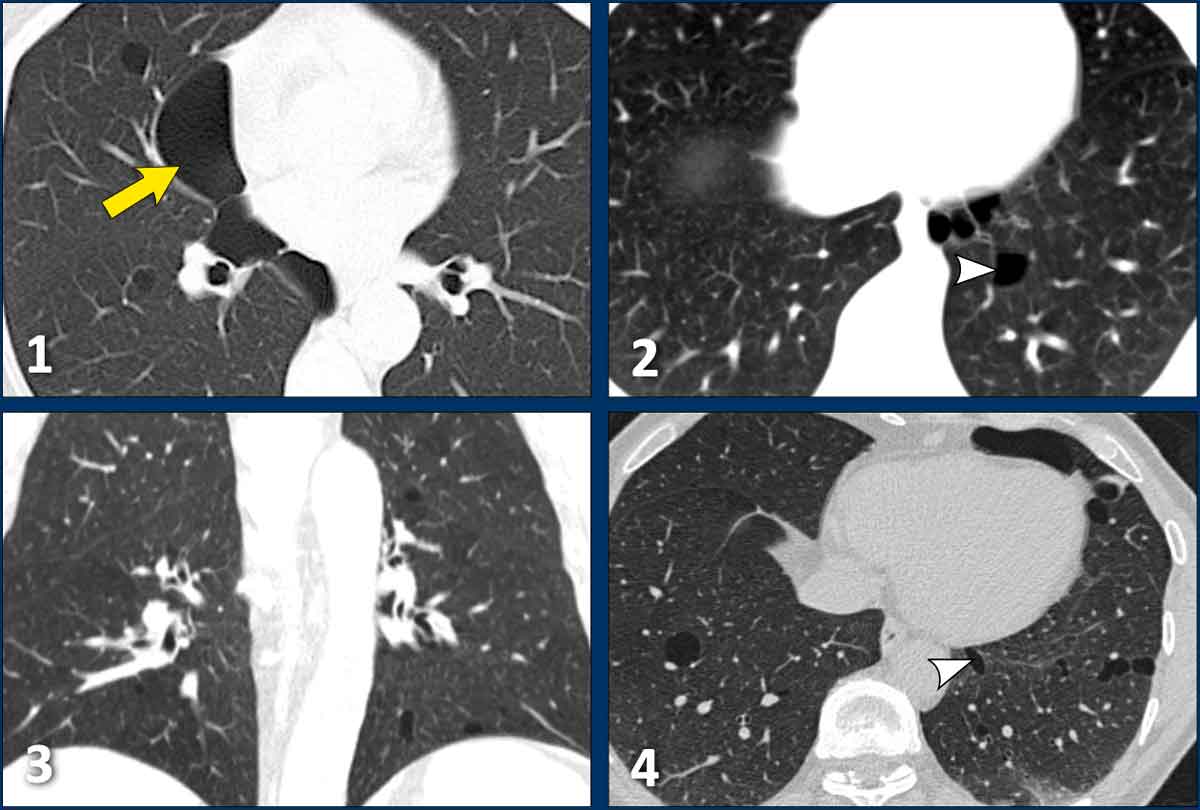
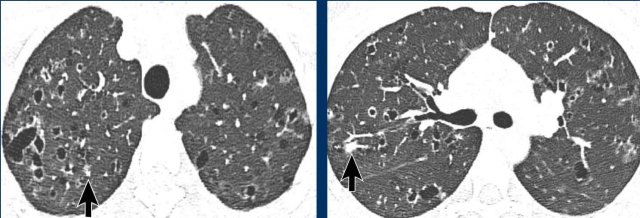
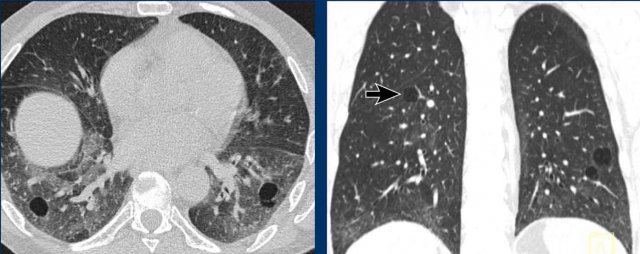
Multiple lesions
When there are multiple findings that look like lung cysts, we should consider next to cystic lung disease also other diseases (figure).
- Multiple lungcysts with fine walls in a patient with LHC. This is a true cystic lung disease.
- Centrilobular emphysema seen as black holes without a wall. Notice central dot sign (arrow). Emphysema can be a real mimicker and we will discuss it in more detail later.
- Honeycombing. Stacks of thick walled cysts in the periphery of the lower lobes in patients with lung fibrosis.
- Cystic bronchiectasis. Cystic tubes. This is usually not a problem as we can scroll through the images.
Step 2 - Is it an incidental finding
In young patients you should not detect any lung cyst as a normal finding.
However as a rule of thumb you can consider up to four cysts in a patient over forty years of age as an incidental finding.
Consider a cystic lung disease when you find more than four cysts or when the patient is suspected of having an interstitial lung disease.
Step 3 - Differential Diagnosis
Nodules
When there are nodular cysts, the most likely diagnosis is LCH, which has a upper zone predominance.
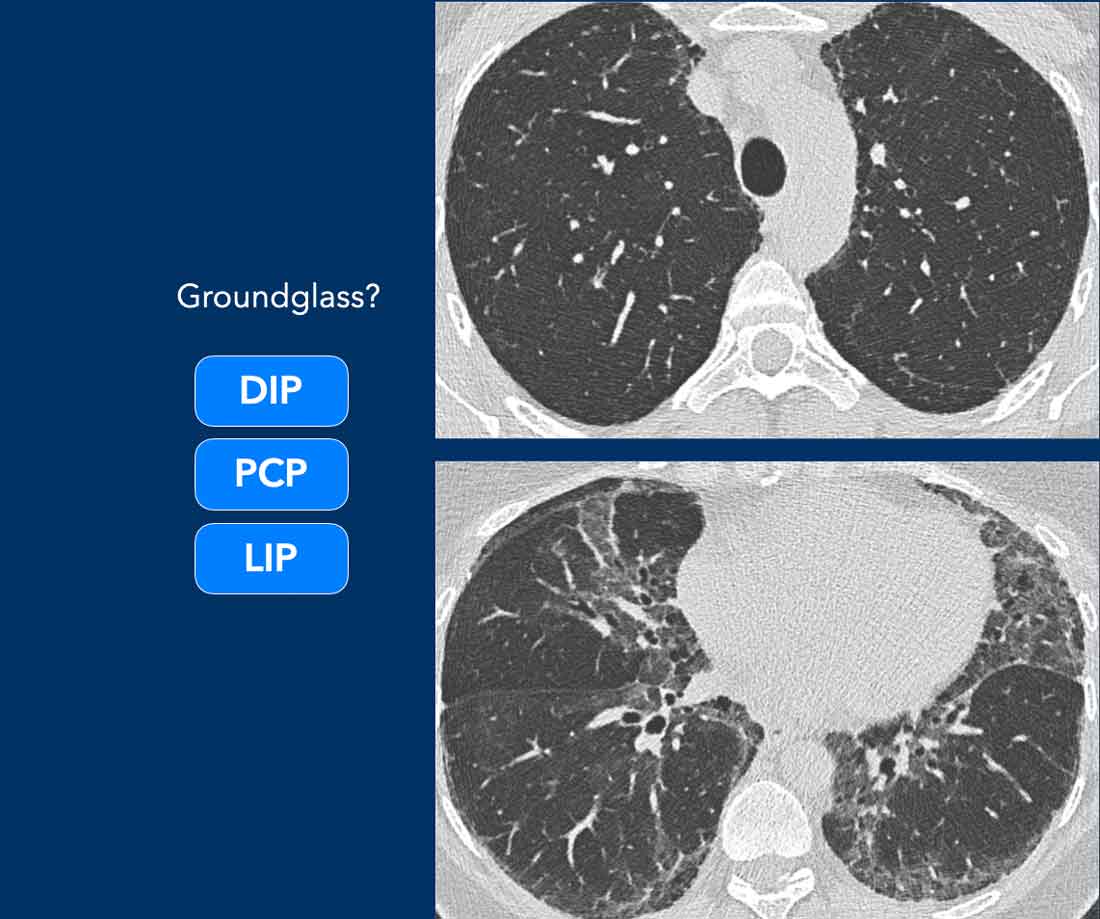
Ground glass
The combination of cysts and ground glass is not common and the most likely diagnosis is LIP.
No nodules or ground glass
Simple cysts without ground glass or nodules are mostly seen in LAM, which is only seen in women.
In men the most likely diagnosis is LCH.
BHD and LIP are less common.
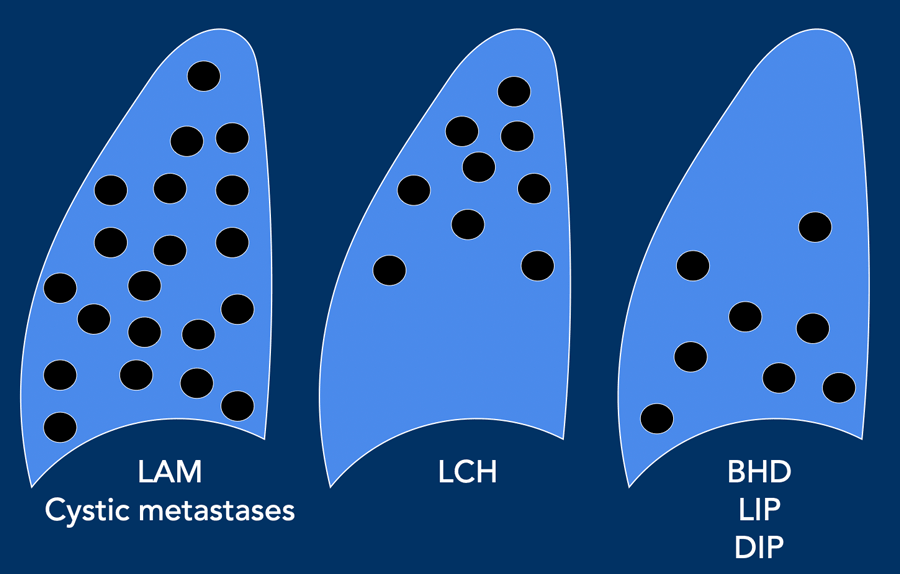
Distribution
The distribution and number of the cysts can be helpful.
- LAM and metastases are usually evenly spread and numerous.
- LCH has an upper lobe preference.
- BHD, LIP and DIP have a lower lobe preference and usually only a few cysts are seen.
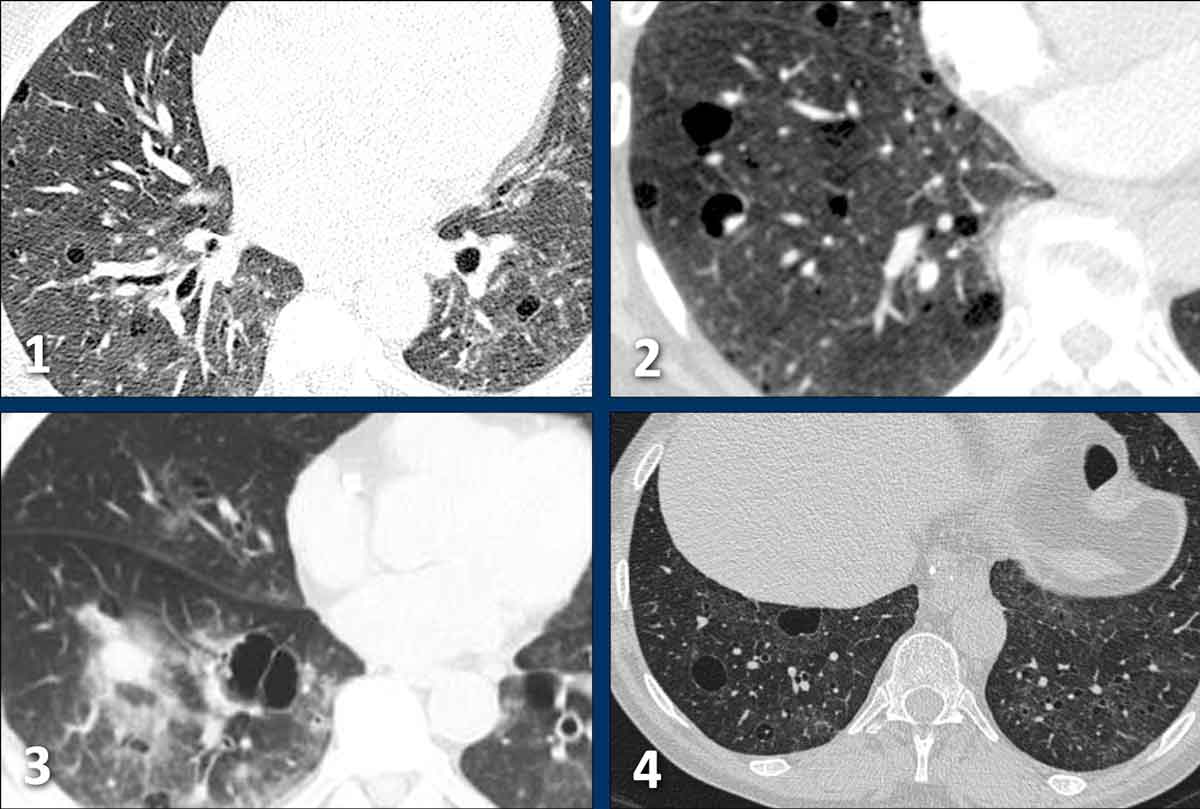
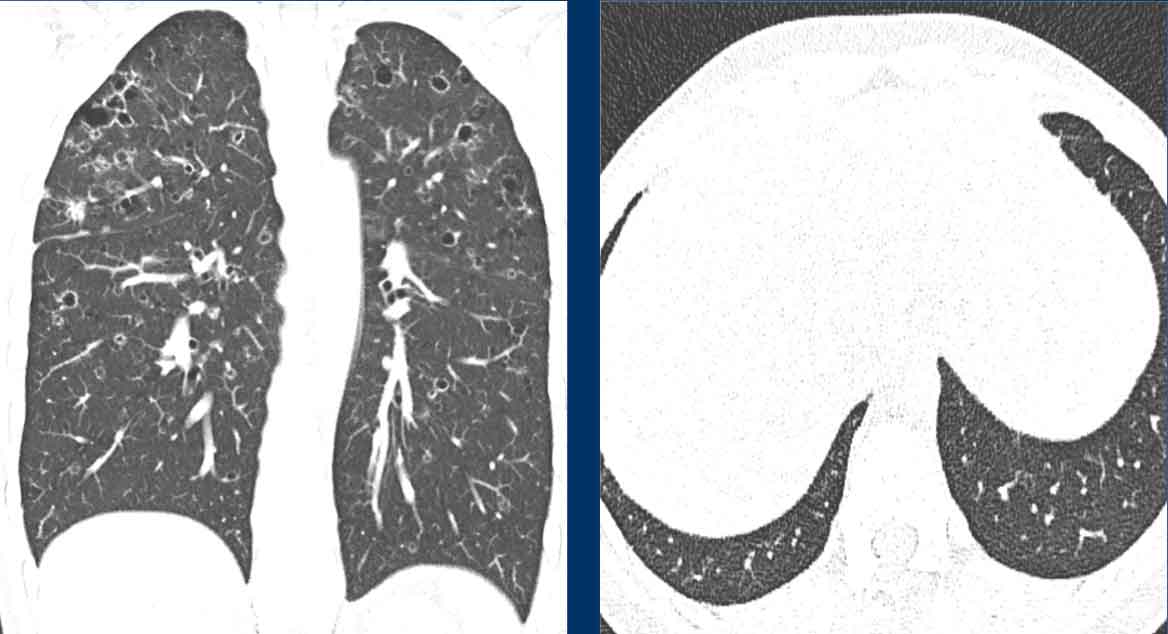
LAM
Lymphangioleiomyomatosis (LAM) is an indolent, progressive disease exclusively seen in young women.
Symptoms are dyspnea, cough, chest pain, and hemoptysis.
Some patients present with spontaneous pneumothorax or pleural effusion.
LAM presents with a large number of round and regularly shaped cysts.
In general, the presence of only simple cysts - regardless of number - should lead to a diagnosis of LAM, except in men when LCH should be considered.
LAM is associated with tuberous sclerosis and the presence of angiomyolipomas.
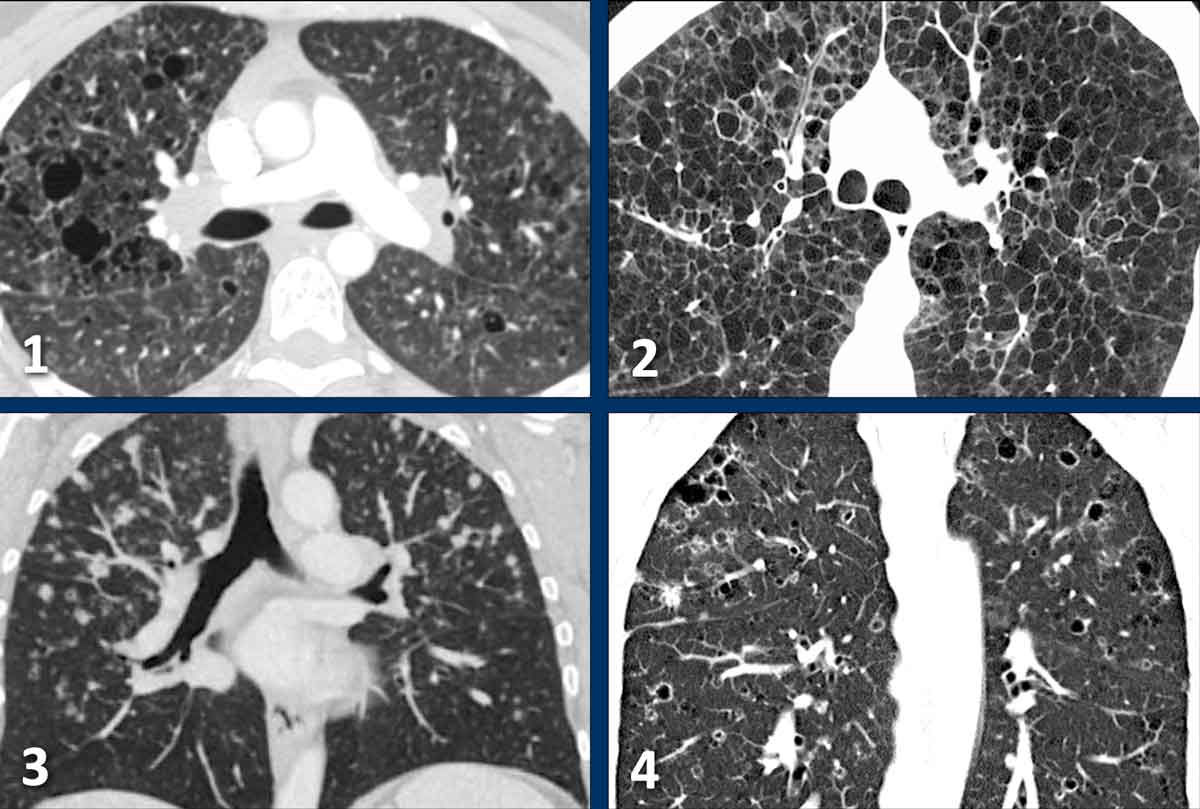
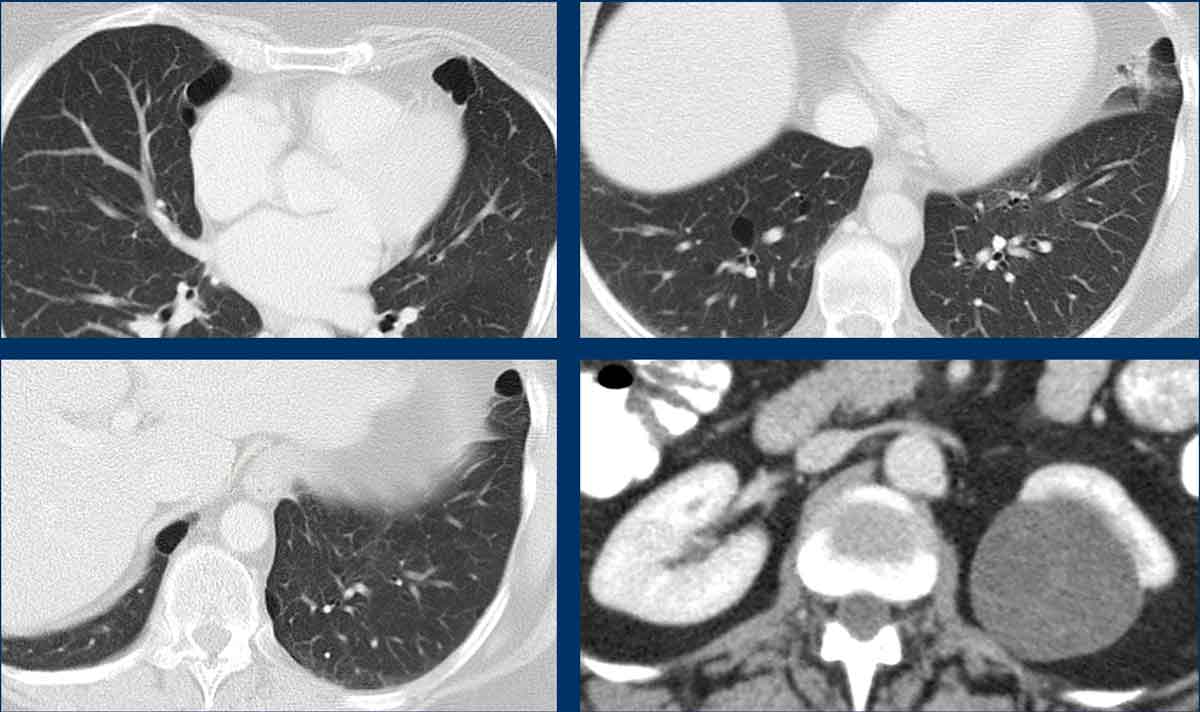
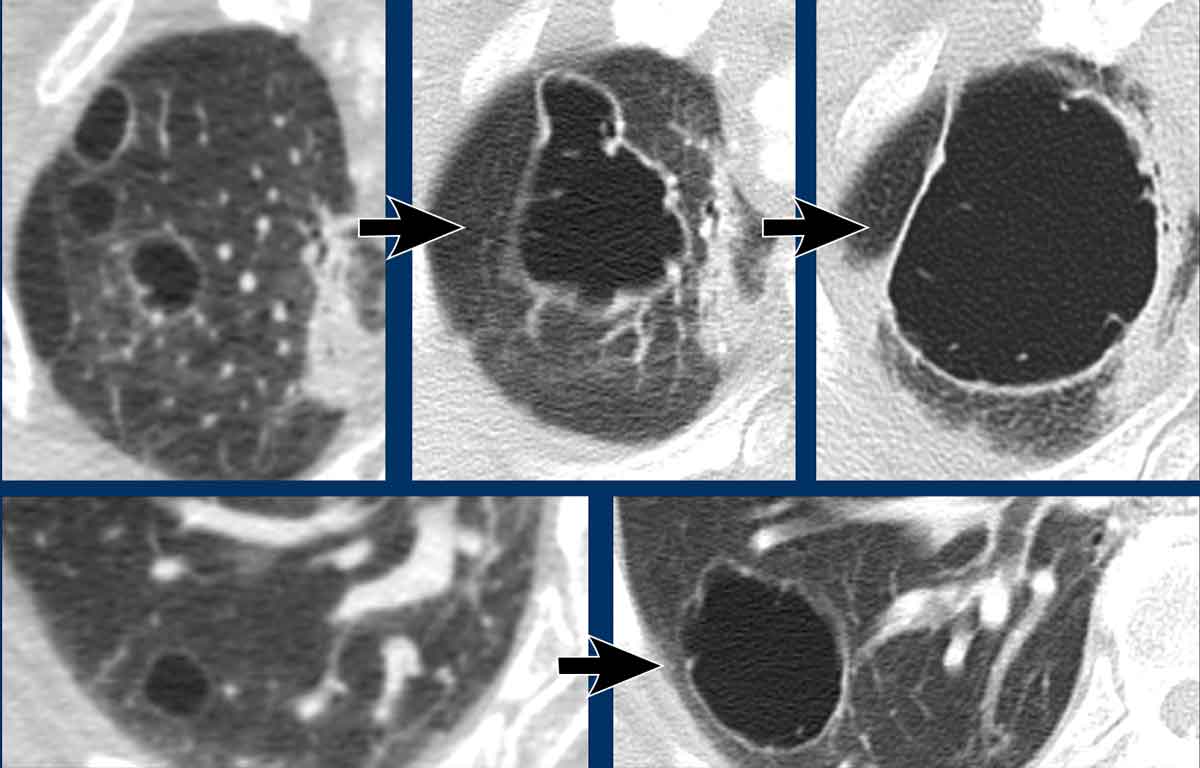
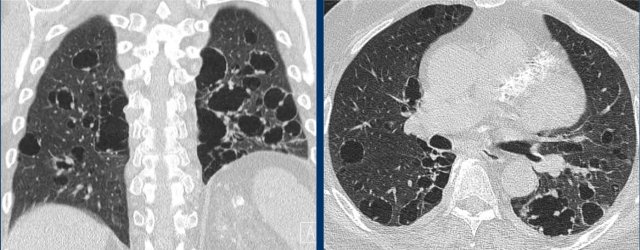
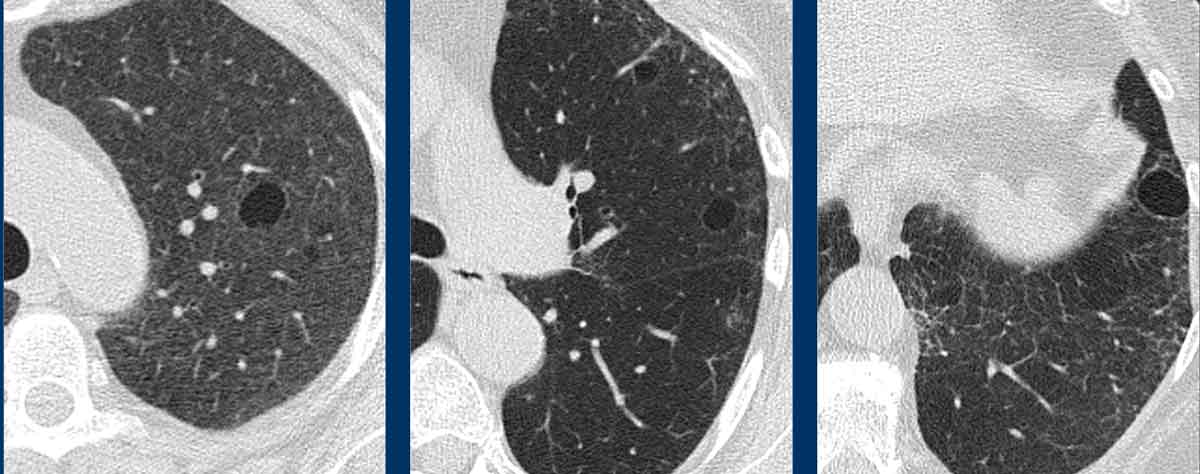
Images
- Numerous cysts in a young woman. Notice the regular round shape and diffuse distribution.
- Severe case of LAM. In men the most likely diagnosis would be LCH.
- Pleural effusion in a patient with LAM.
- Diffuse distribution in LAM.
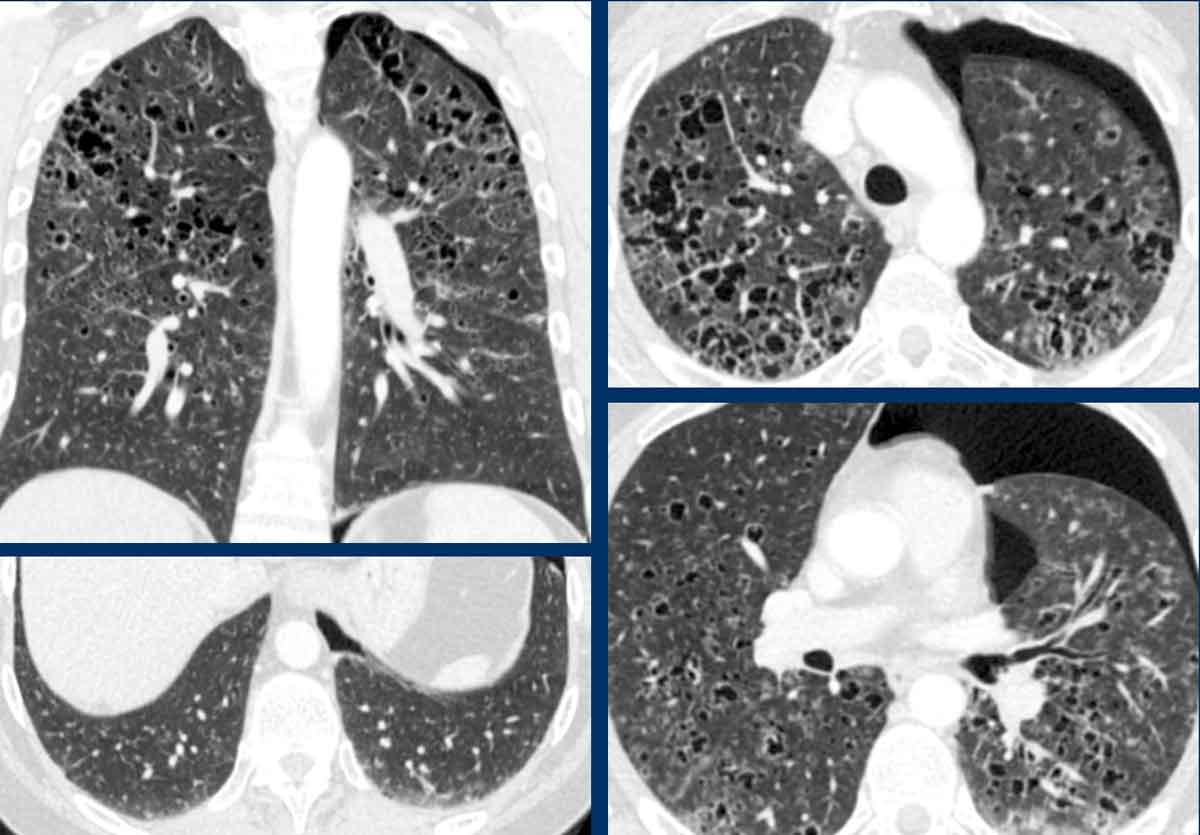
LCH
The etiology of Langerhans cell histiocytosis is unknown, but cigarette smoking plays a primary role.
Patients are at increased risk of lung cancer.
LCH starts as nodules, that cavitate and transform into cysts with irregulars forms (bizarre cysts).
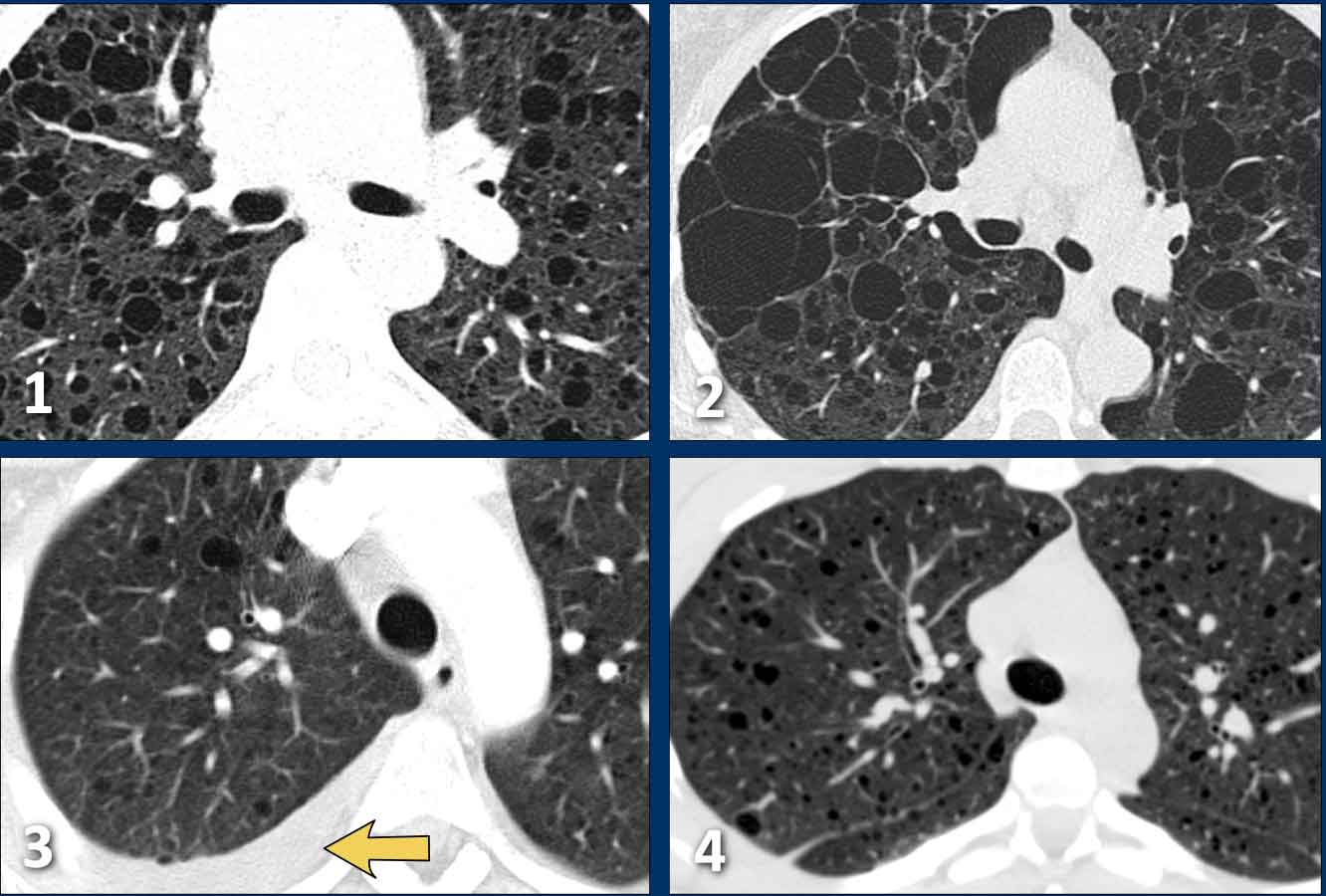
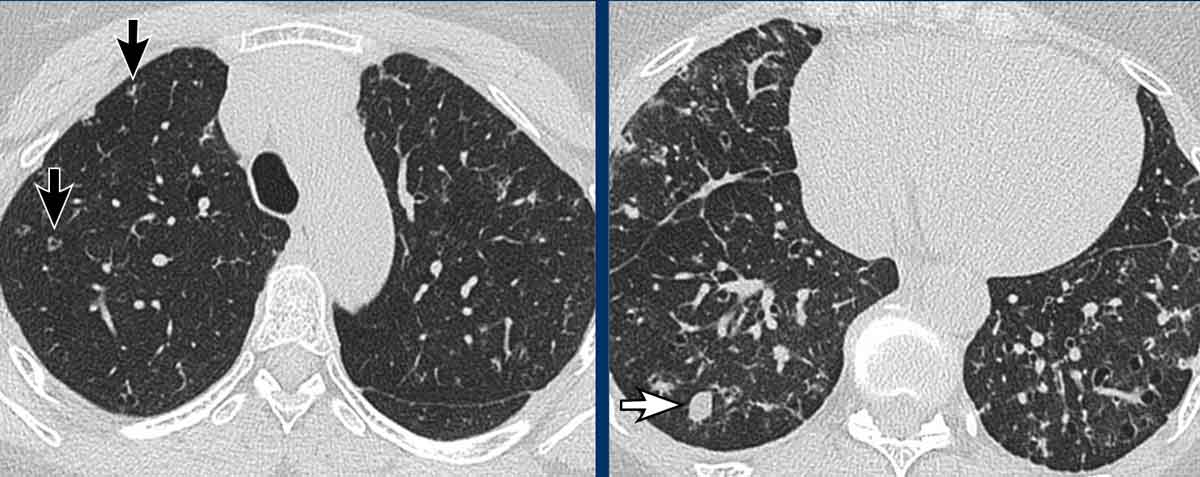
Images
- Bizarrely or irregularly shaped cysts in a man with LCH.
- Extreme case of LCH almost resembling honeycombing.
- Multiple nodules with an upper zone predominance (unlike metastases).
- Bizarre shaped cysts with upper zone predominance
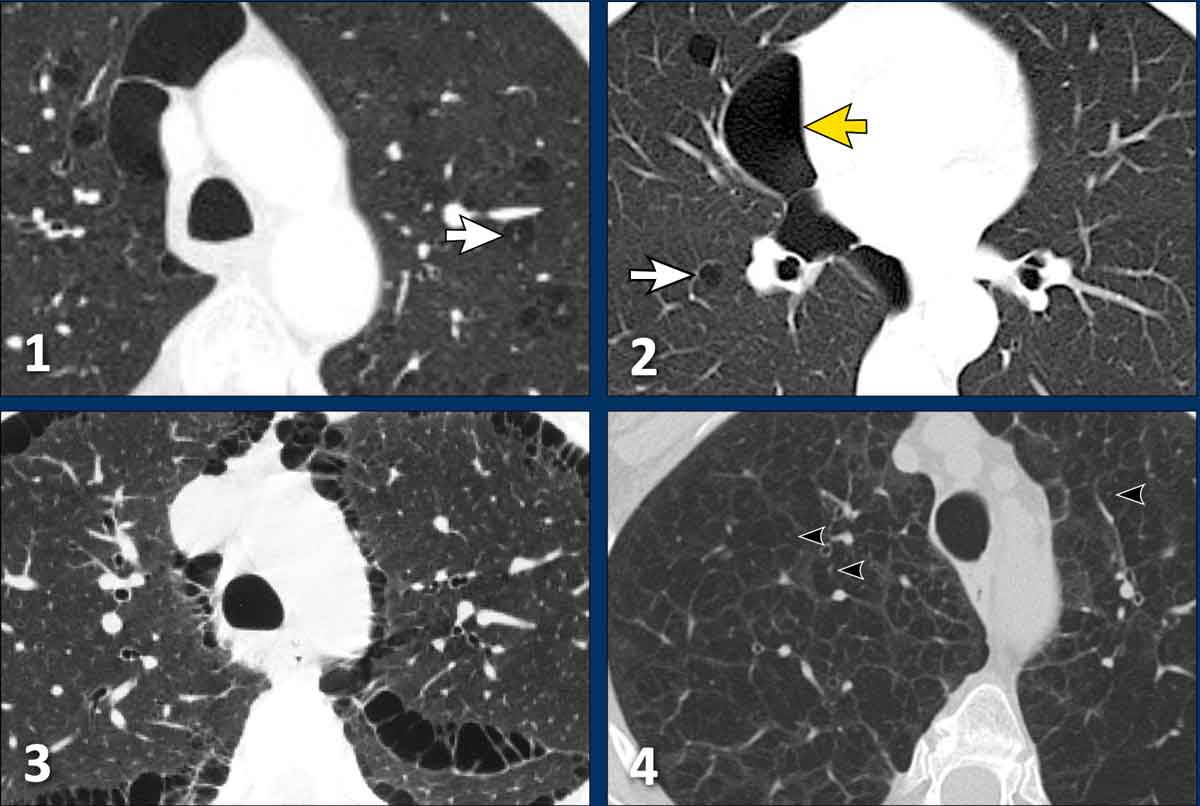
BHD
Birt-Hogg-Dubé syndrome is a genetic disorder with a 25% risk of renal cancer.
The cysts in the lungs can cause recurrent pneumothorax.
BHD cysts sometimes have some borders defined by interlobular septae giving them a triangular or lenticular shape (arrowheads in 2 and 4).
BHD cysts are not numerous, usually less than 50 cysts.
BHD-cysts have a lower field predominance.
It is important to make the diagnosis because these patients and their family need to be screened for renal tumors.
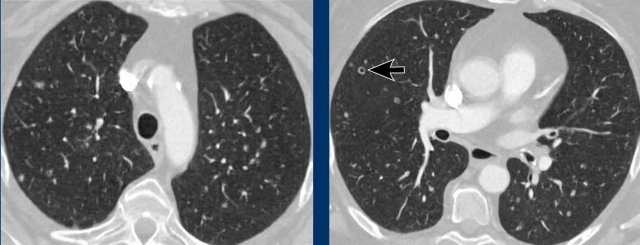
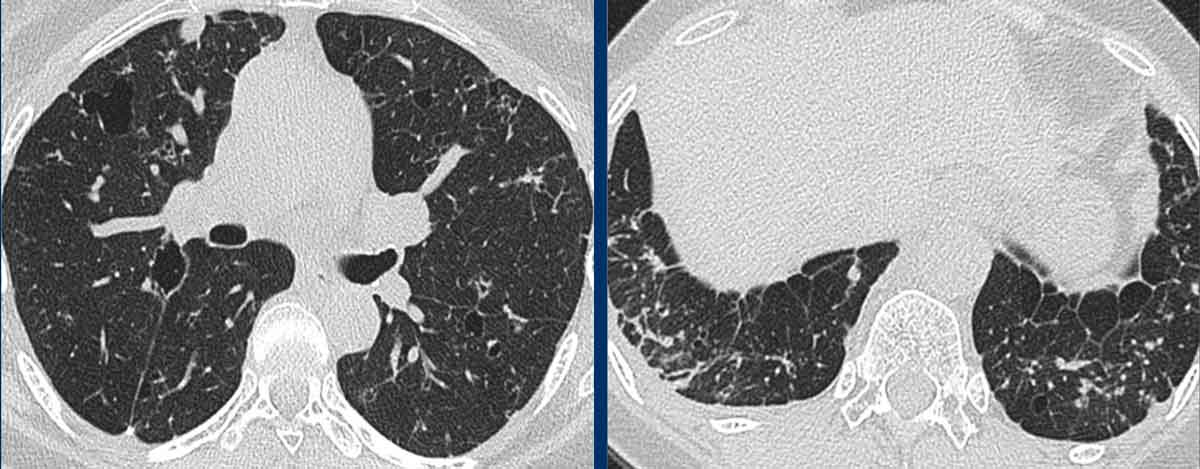
Images
- BHD cysts. Some are adjacent to the pleural (yellow arrow). Peri-pleural cysts may also be seen in LIP and both have a lower zone predominance.
Paraseptal emphysema is upper zone predominant. - Lower zone predominance and triangular shape (arrowhead)
- Notice the lower zone predominance.
- Typical BDH cysts
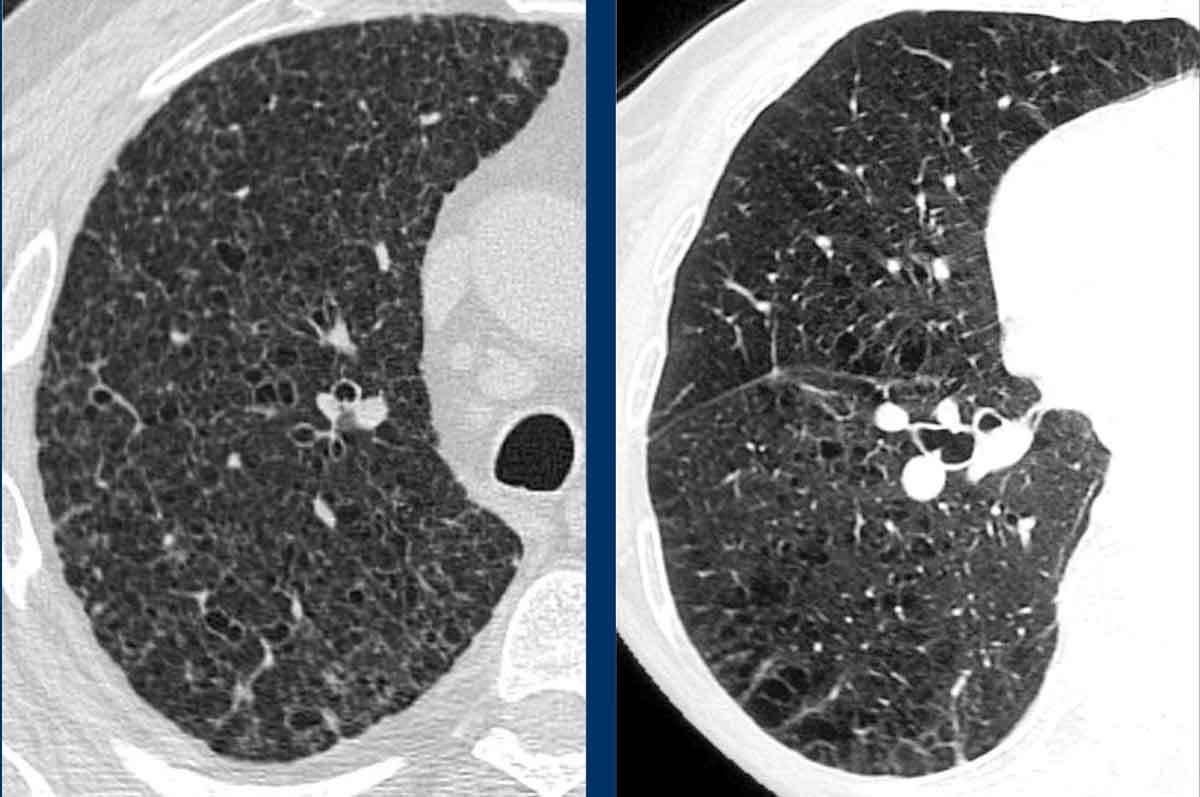
LIP
Lymphoid interstitial pneumonia is an interstitial lung disease of unknown etiology, that is characterized by infiltration of lymphocytes.
It is associated with systemic diseases (especialy M. Sjögren).
It can present as only simple cysts or in combination with ground glass, reticulation and noduli.
Images
- Simple cysts in diffuse ground glass.
- Simple cysts in LIP. Sometimes you can see vascular indentations.
- Simple cysts in an area of ground glass.
- Simple cysts.
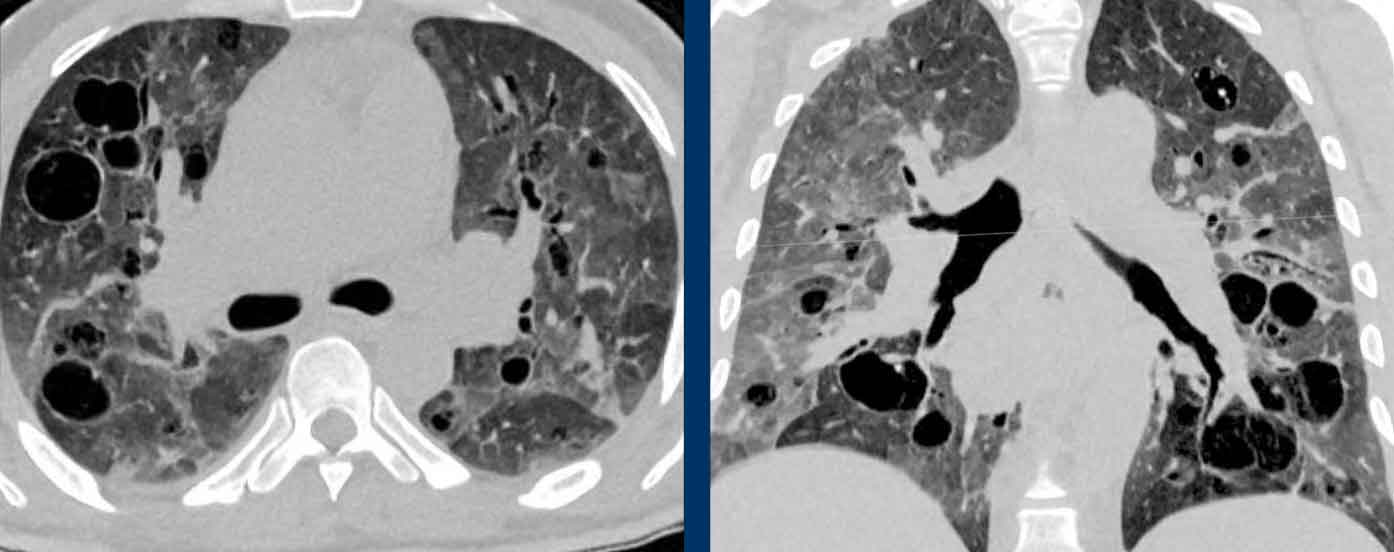
Emphysema
Some examples of emphysema are included here because emphysema can sometimes simulate a cystic lung disease.
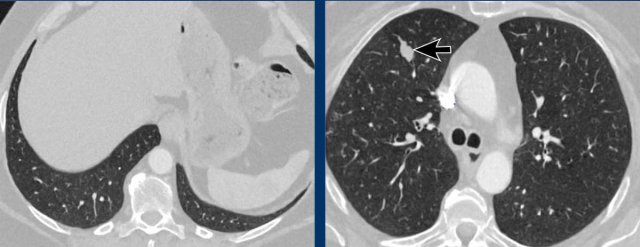
Images
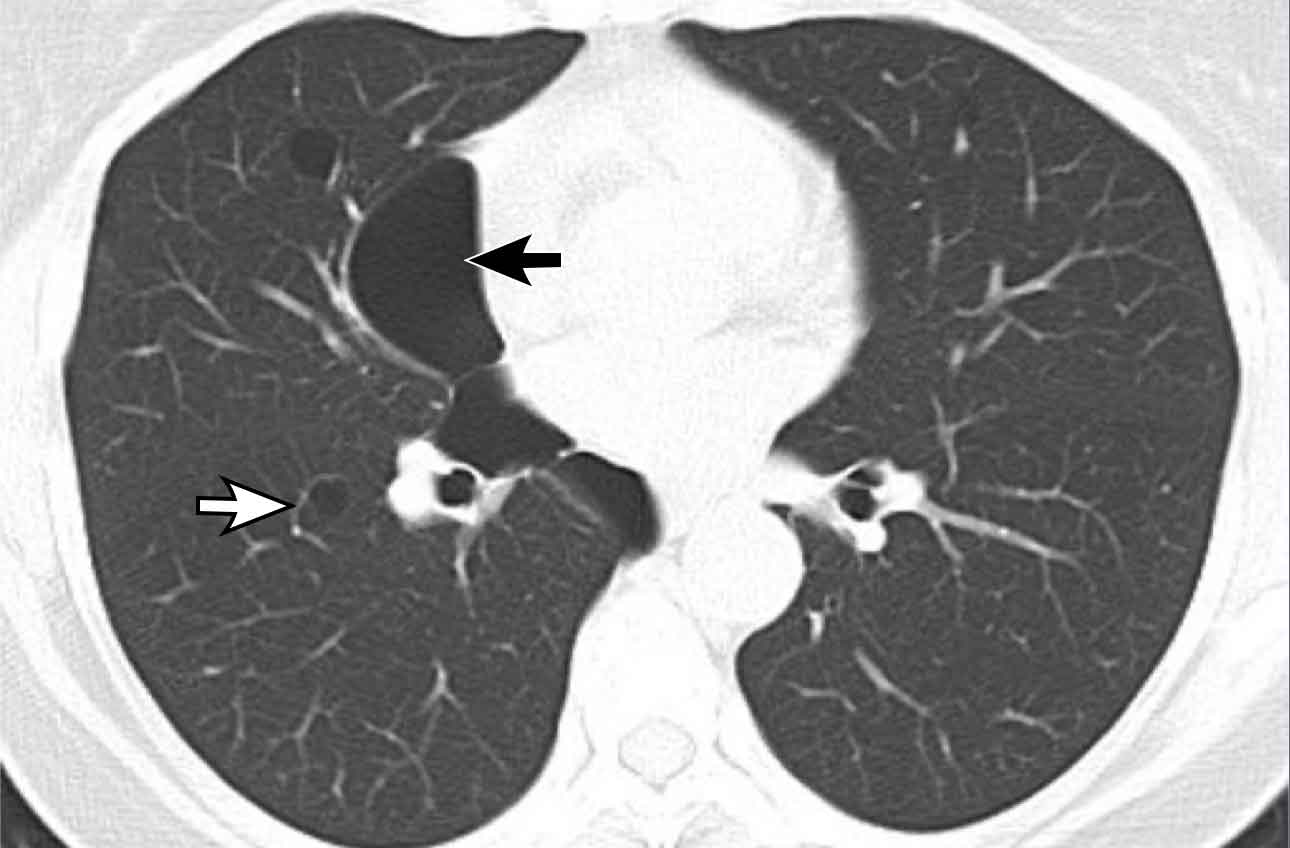
- Centrilobular emphysema with central dot sign (white arrow) and paraseptal emphysema. Notice the resemblance to 2.
- This is not emphysema but a Birt-Hogg-Dubé case with simple cysts in the lung parenchema and paraseptal cysts.
- Paraseptal emphysema.
- Centrilobular emphysema with central dot sign (black arrowheads).
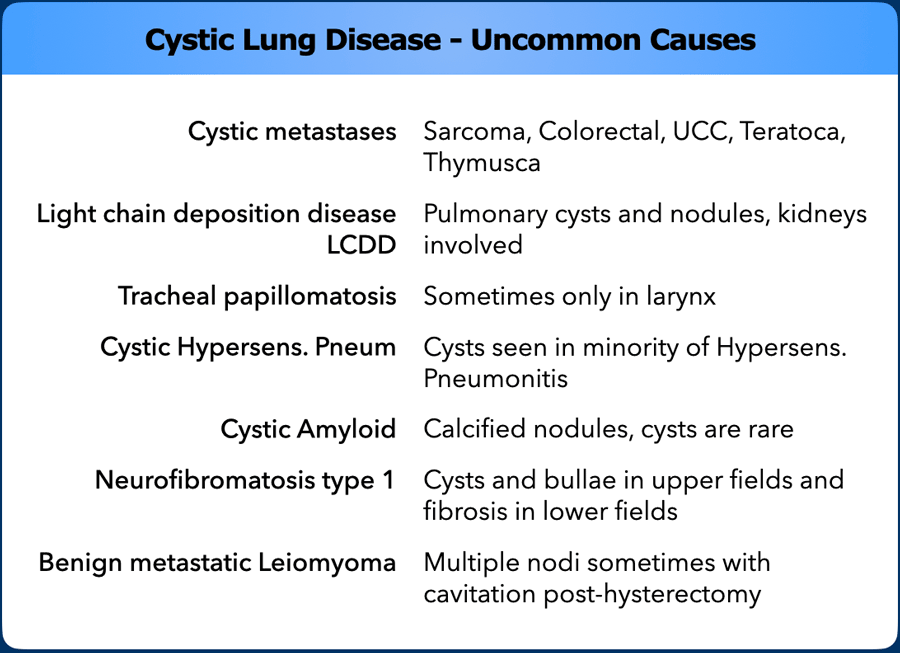
When the cysts do not fit into the diagnosis of the usual suspects (LAM, BHD, LCH, LIP), then think of uncommon causes of cystic lung disease.
Solitary cyst - Study cases
In this chapter we will show you some cases of solitary cysts.
Use the diagnostic approach and try to come up with a differential diagnosis.
Case 1
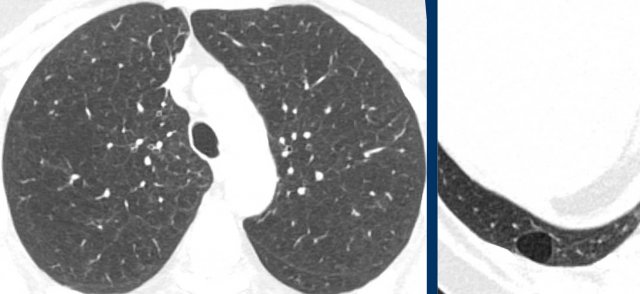
These images are of a 67-year-old woman with a history of scleroderma, who quit smoking twelve years ago.
She now has a HRCT.
Study the images.
Is this a lungcyst or mimicker and what is the most likely diagnosis?
Findings
In the right lower lobe is a true cyst with a nice thin wall without any irregularities.
Discussion
This is regarded as an incidental cyst without any clinical meaning.
These incidental cysts are usually located in the periphery of the lower lobes.
Case 2
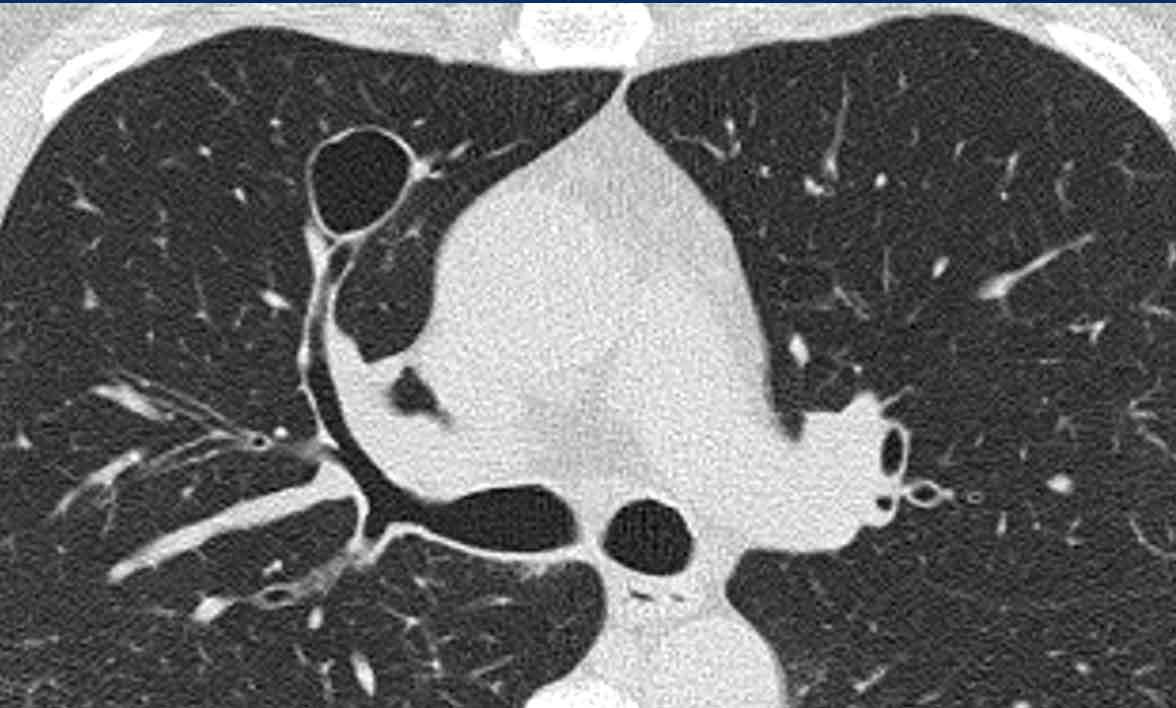
These images are of a 58-year-old man.
He has periods of productive coughing especially when he was lying on his left side.
No smoking history.
Study the images.
Is this a lungcyst or mimicker and what is the most likely diagnosis?
Findings
There is a cyst in the right upper lobe and this was the only cystic structure in the lungs.
Discussion
You could think of an incidental cyst, but that is unlikely, because an incidental cyst cannot explain the coughing.
It was decided to do a follow up scan
Continue with the next images...
The image after six months shows something that looks like wall thickening and a PET-CT was performed to look for any sign of malignancy.
The PET scan was negative and further follow up was done and an air-fluid level was seen.
This finding together with the approximity to the bronchus made the diagnosis of a bronchogenic cyst the most likely.
Because persistent complaints, the cyst was removed and the diagnosis was confirmed.
The periods of coughing were thought to be the result of infected material within the cyst emptying into the bronchial tree.
Bronchogenic cysts are congenital malformations that have lost the normal connection to the bronchial tree and usually are filled with fluid.
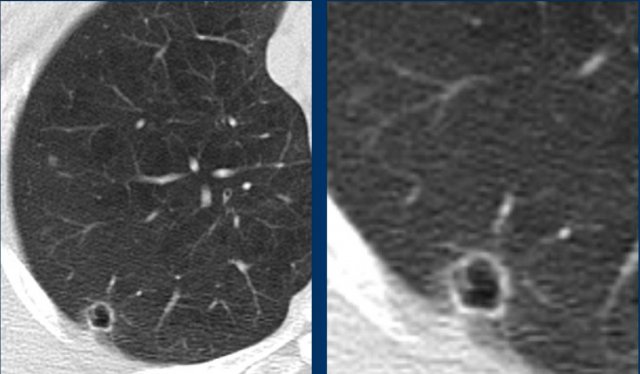
Case 3
This image and detail are of a 56-year-old woman who was treated for a papillary thyroid cancer.
There was a follow up scan that showed a solitary cyst-like lesion.
Study the image.
Is this a lungcyst or mimicker and what is the most likely diagnosis?
Findings
There is centrilobular emphysema and an air-filled lesion with an irregular wall.
Discussion
Our mayor concern is a cystic lungcancer.
A solitary metastasis of the thyroid cancer is less likely since widespread multiple metastases are far more common.
Continue with the next images...
On a scan one year earlier a small area of ground-glass was detected at the same location and at that time a PET-CT was performed which showed only minimal activity.
What do we do with this information?
Continue...
The diagnosis of a cystic lung cancer was still high on our list and it was decided to continue the follow up.
Although the wall becomes less irregular, this should not be regarded as a sign of benignity.
It is probably the result of progressive necrosis.
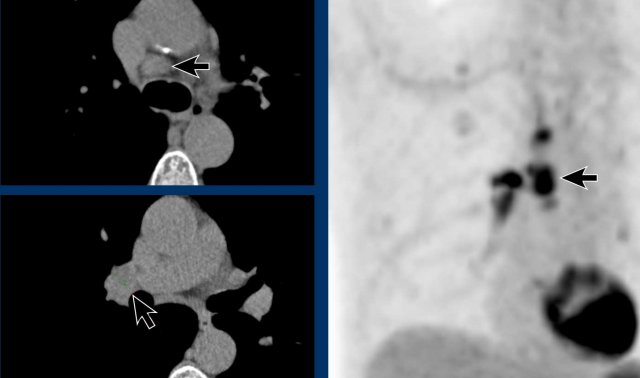
In 2019 a new PET-CT was performed which again showed only minimal activity.
This also should not reasure you.
It can be explained by the minimal solid component.
Continue...
The 2019 PET-CT however also showed positive hilar and mediastinal lymph nodes (arrows).
Final diagnosis
Metastatic non-small cell lung cancer.
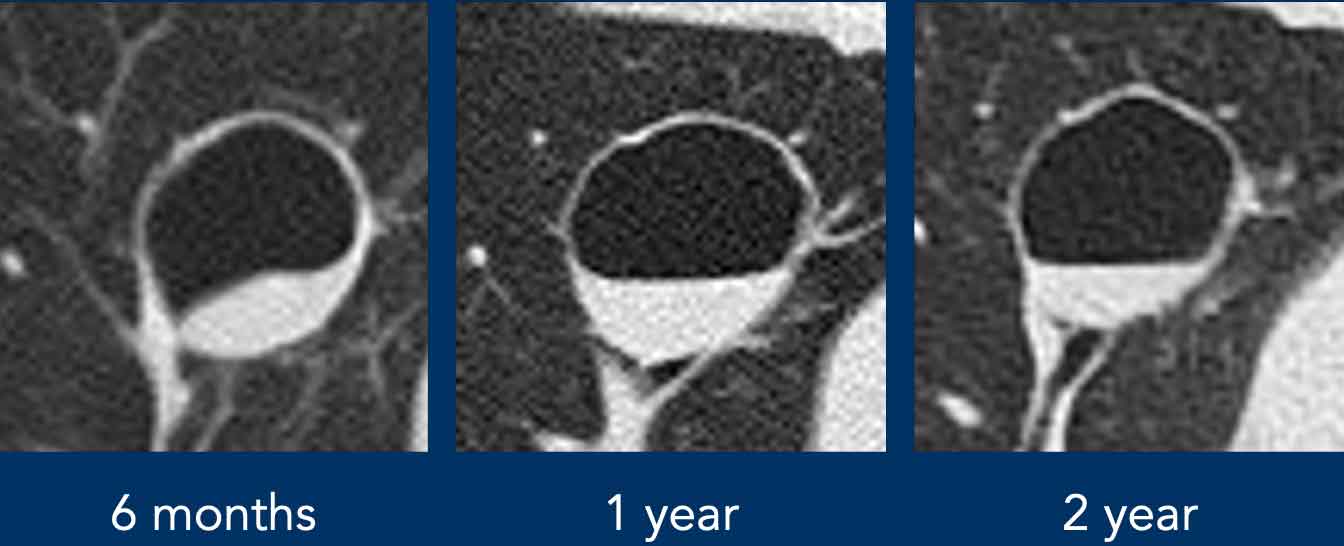
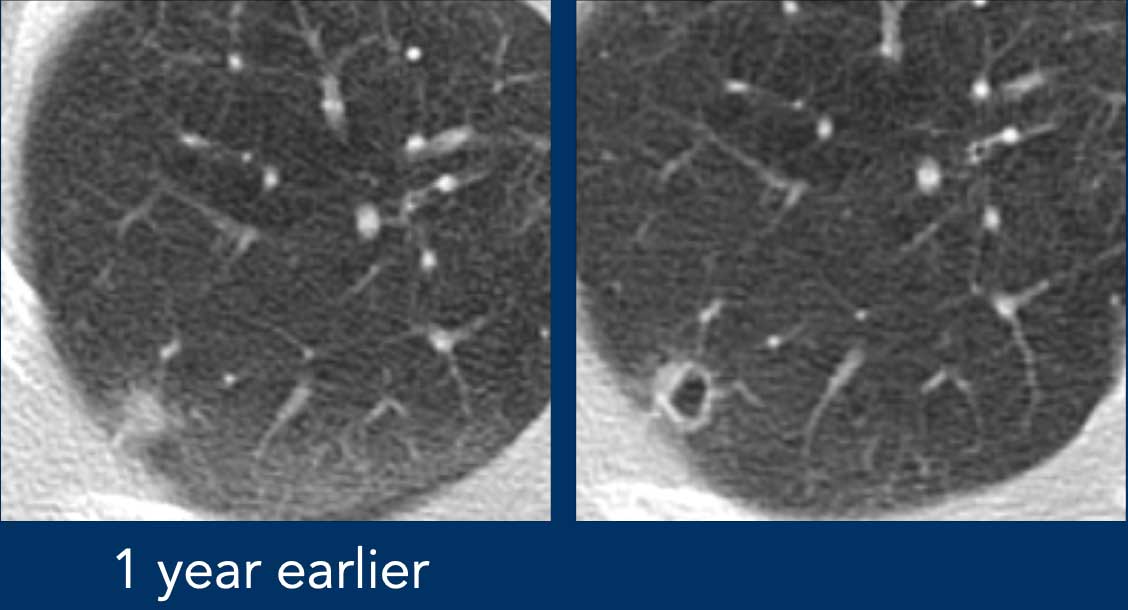
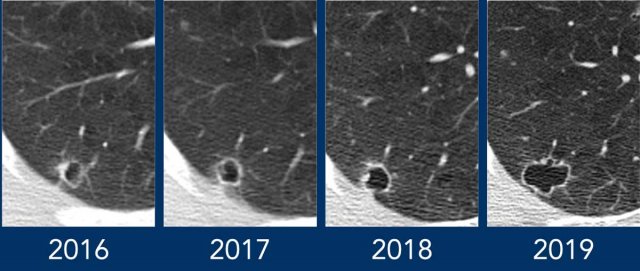
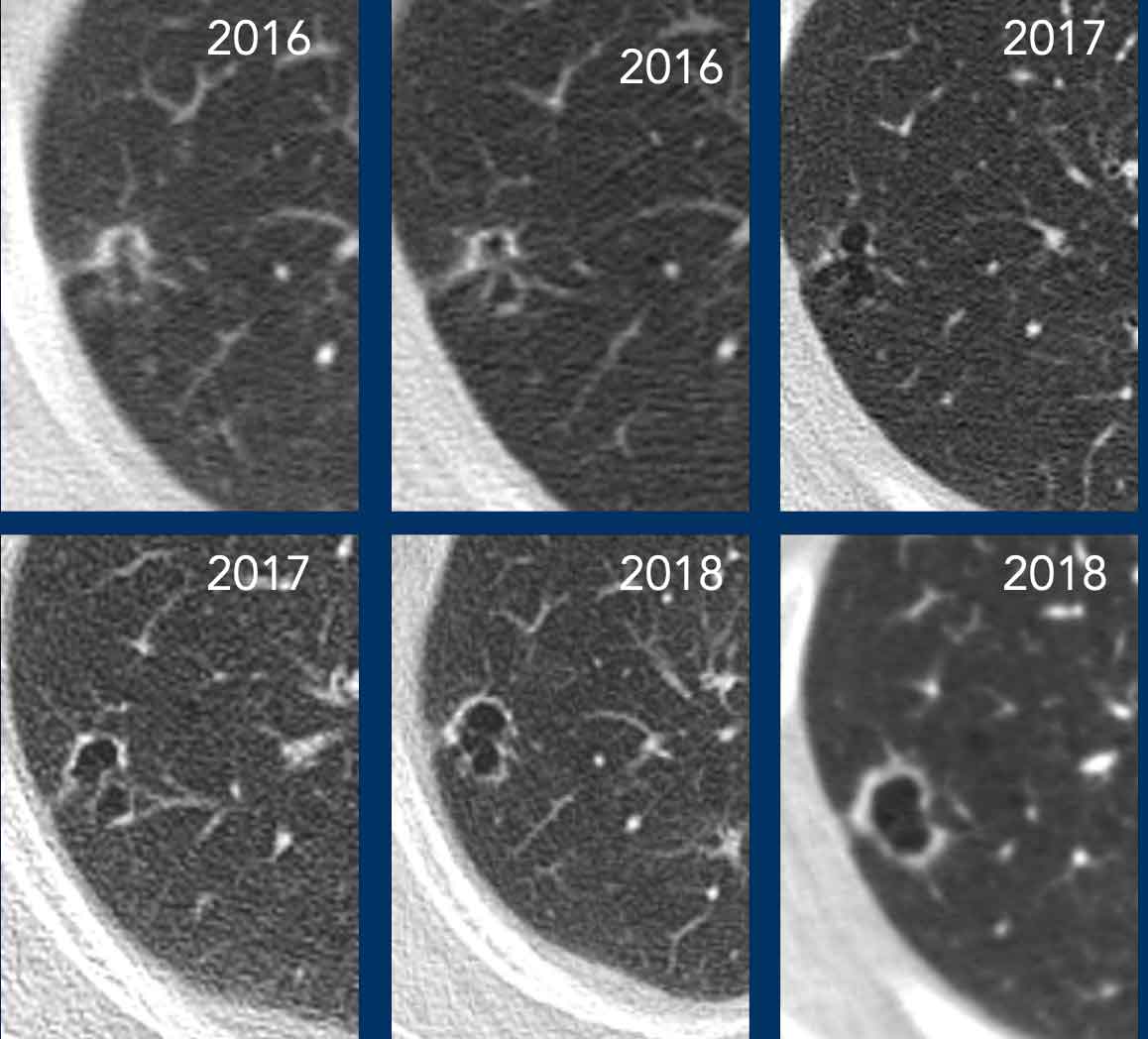
Case 4
Here a similar case.
This is a 64-year-old woman who was treated for breastcancer.
In 2016 there is a slightly thickened wall.
In 2017 however the wall is more regular and not thickened.
In 2018 the lesion enlarges and the wall again becomes thickened.
This also proved to be lung cancer and luckily surgery proved to be curative.
Read more about cystic lung cancer on the Radiology Assistant in the article of Onno Mets.
Multiple cysts - Study cases
Use this table when you want to differentiate lung diseases with multiple cysts.
If it is not one of the more common cystic lung diseases, think of uncommon causes.
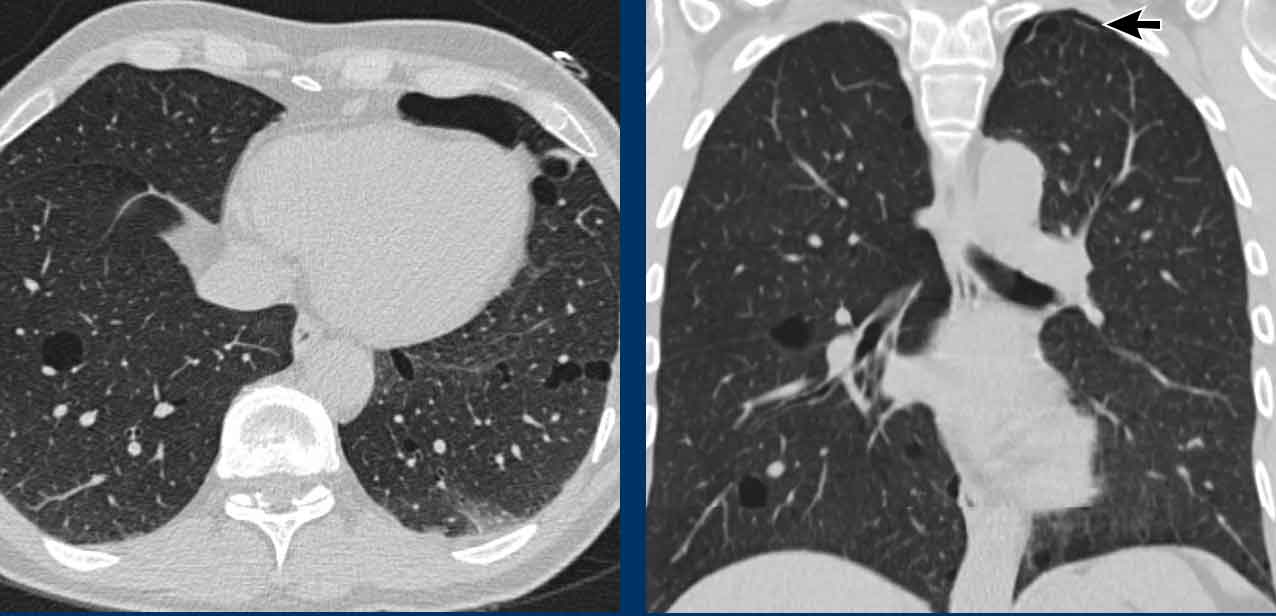
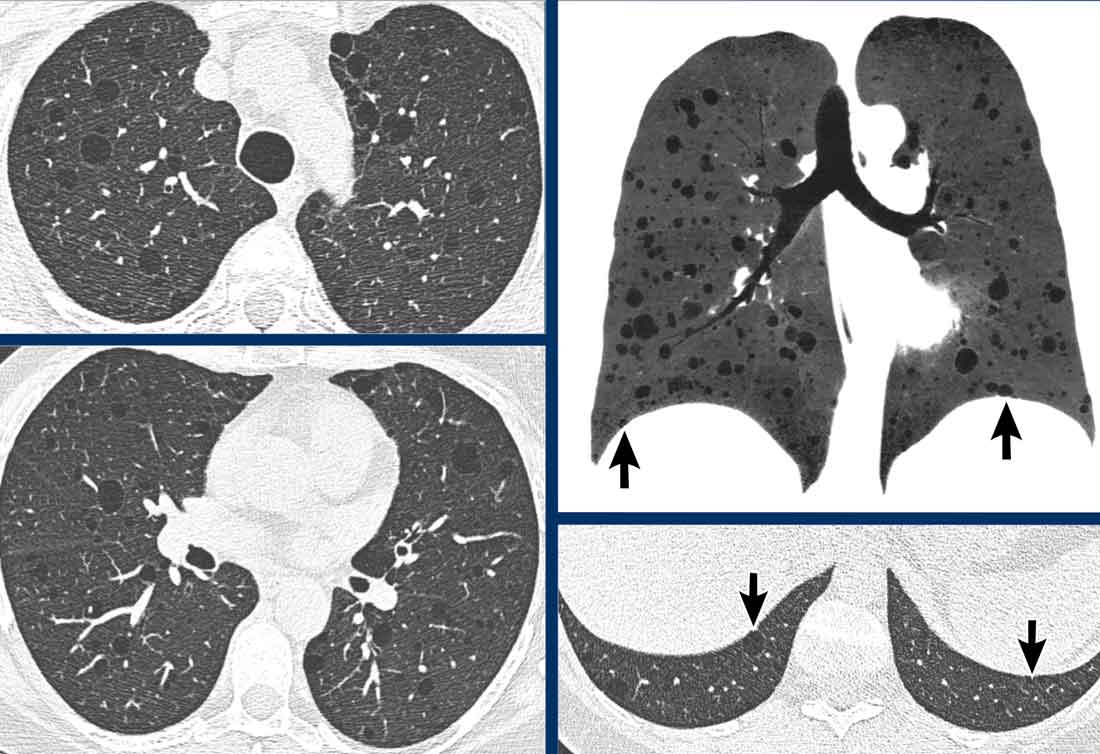
Case 1
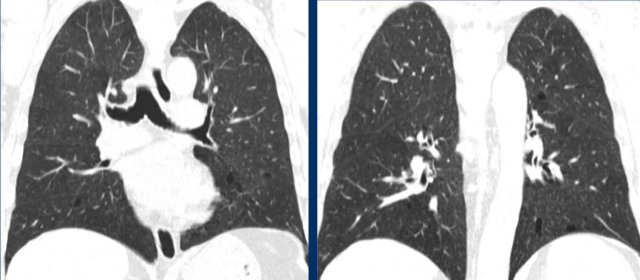
These images are of a 56-year-old man, who had recurrent pneumothorax and now agin presents with a pneumothorax (arrow).
Study the image.
Are these cysts or mimickers? Is this an incidental finding or do you think it is a cystic lung disease.
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts - more than four. Notice the localisation near septa in the periphery of the lung.
Discussion
The two cystic lung diseases, that frequently present with a pneumathorax, are LAM and Birt-Hogg-Dube syndrome (BHD).
LAM presents as simple cysts, which are thin walled, round or oval and regularly shaped.
BHD cysts have some borders defined by interlobular septae (arrows). The peri-septal location often gives the cysts sharp angles that causes them to have a lenticular shape.
When cysts have this typical appearance, they have a extremely high specificity for the diagnosis of Birt-Hogg-Dube syndrome.
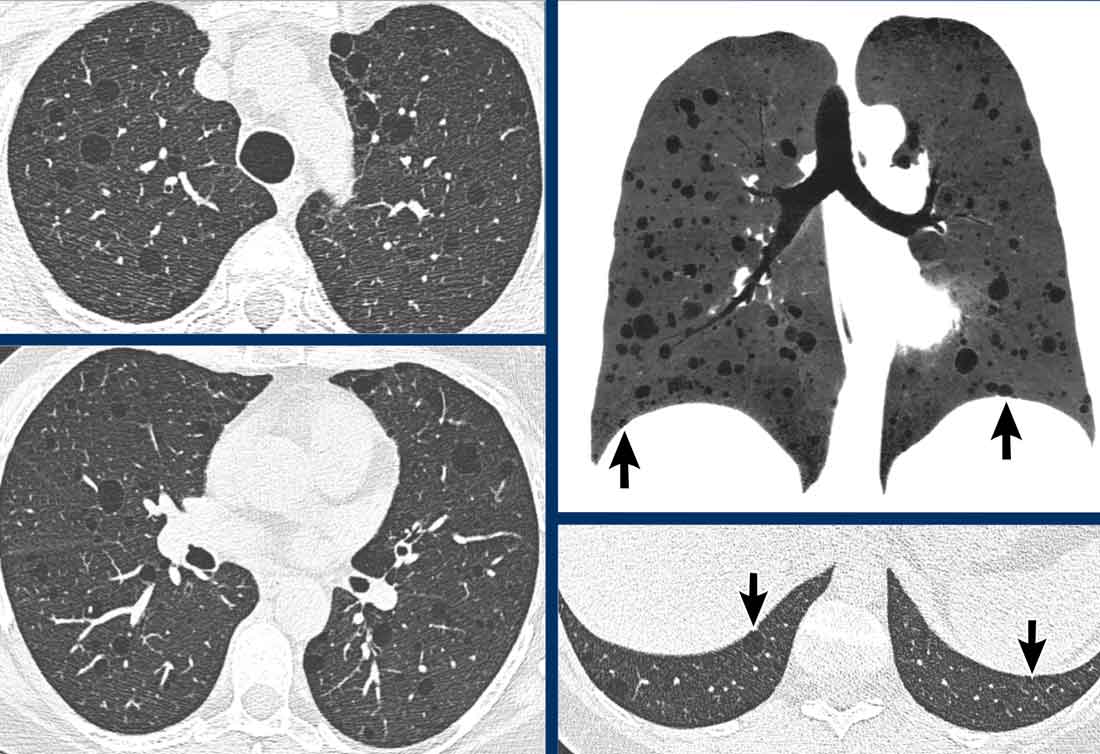
Case 2
These images are of a 39-year-old woman with dyspnoe.
Study the image.
Are these cysts or mimickers? Is this an incidental finding or do you think it is a cystic lung disease.
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts. Notice that the cysts are evenly spread throughout the lungs.
Discussion
The pleural sinuses are also involved (arrows).
This means that we can skip diagnoses like LCH and emphysema.
In general, the presence of only simple cysts - regardless of number - should lead to a diagnosis of LAM, except in men when LCH should be diagnosed.
Case 3
This is another case of BHD.
The cysts are typically located peripheral in the lower lobes like in this case.
One of the cysts is near the fissure (white arrow).
The paramediastinal cysts (black arrow) are also peripheral in location.
Sometimes you need to study the lung fields very carefully not to overlook the cysts and miss the diagnosis of Birt-Hogg-Dube syndrome.
In this case you can imagine, that if the CT is performed for another reason, that you van easily miss these tiny cysts.
Remember that when you see more than four cysts and they are truly cysts, you need to do something with the findings.
These patients should go to a pulmonologist for further work up.
Case 4
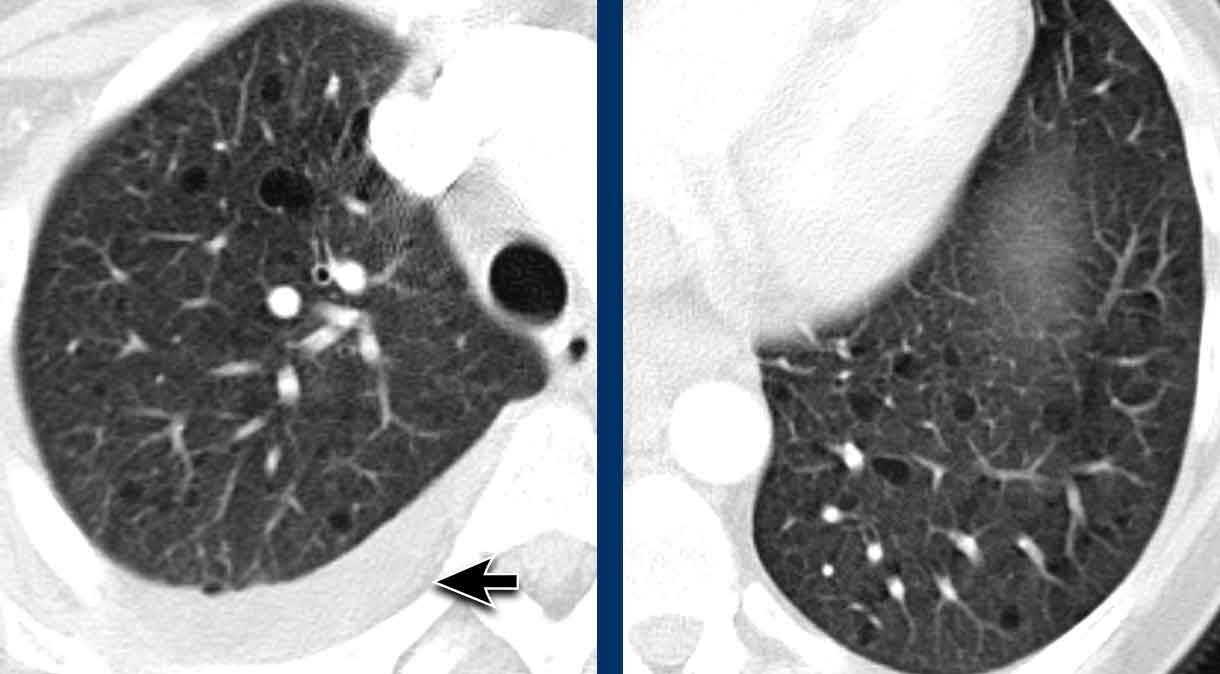
These images are of a 43-year-old woman with dyspnoe.
Study the image.
Are these cysts or mimickers?
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts. The cysts are evenly spread throughout the lungs.
There is a pleural fluid collection on the right (arrow).
Discussion
The presence of only simple cysts ina woman should lead to a diagnosis of LAM.
LAM is the only cystic lung disease in which we can see the combination of cysts and pleural fluid.
LAM cells may lead to blockages of the lymph system in the chest and create a chylous pleural effusion.
later it became clear, that his patient was known with tuberous sclerosis and multiple angiomyolipomas.
Case 5
These images are of a 60-year-old woman with Sjögren's disease, who had a HRCT to screen for interstitial lung disease.
Study the image.
Are these cysts or mimickers?
What is the most likely diagnosis?
Findings
There are a few cysts, but also on other images (not shown) it turned out to be more than four, so we are dealing with a cystic lung disease. There is some ground glass in the lower lung fields and some reticulation as a result of thickened interlobular septa.
Discussion
The combination of cysts and ground-glass limits the differential diagnosis to LIP, DIP and cystic PCP.
In a patient with Sjögren's disease, the diagnosis is LIP.
Case 6
These images are of a 66-year-old man, who is a smoker and complaints of dyspnoe.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
There are multiple cysts. Some are irregularly shaped and some have a cheerio sign (white arrows). There are also some nodules (black arrows).
Discussion
The combination of these findings in a smoker is typical for the diagnosis LCH.
Continue...
Notice that the cysts predominantly involve the upper and middle lobes with relative sparing of the lung bases.
Especially when LCH is still in the nodular phase, this distribution can be a helful sign in the differentiation of metastases, which have a lower lobe preference.
Here a similar case.
Notice that the cysts predominantly involve the upper and middle lobes>
The pleural sinuses are spared.
Case 7
These are images of two different patients.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
Although at first glance these images look similar, you may notice that on the left we have true cysts with a wall in a patient with LCH, while on the right some appear to have a wall, but most of them do not.
This is centrilobular emphysema.
Case 8
This patient had a CT for work up of a renal tumor.
In the radiology report the cysts in the lungs were described as bullae.
These cysts however are typical BHD-cysts in the periphery of the lungs, while bullae are seen in patients with emphysema and are located in the upper lung fields.
Especially when you only see a few cysts, then think of BHD.
The family need to be screened for BHD-syndrome and renal tumors.
Case 9
These images are of a 59-year-old woman with a history of rectal cancer.
Her previous chest-ct was normal.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
There are multiple nodules and some of them show cavitation (arrow), which gives them the appearance of thick-walled cysts.
Discussion
The most likely diagnosis is metastases.
Is there anything that you want to know?
Continue...
You wanna look at the pleural sinuses.
In this case there are no nodules in the pleural sinuses.
This is uncommon in metastatic disease.
At another level a mass was detected, which was biopsied and proved to be a carcinoid.
This was a coincidental finding, but luckily LCH was also found in the biopsy specimen.
Notice that the carcinoid is near a bronchus and that there is air-trapping. Both findings are typical of carcinoid.
Case 10
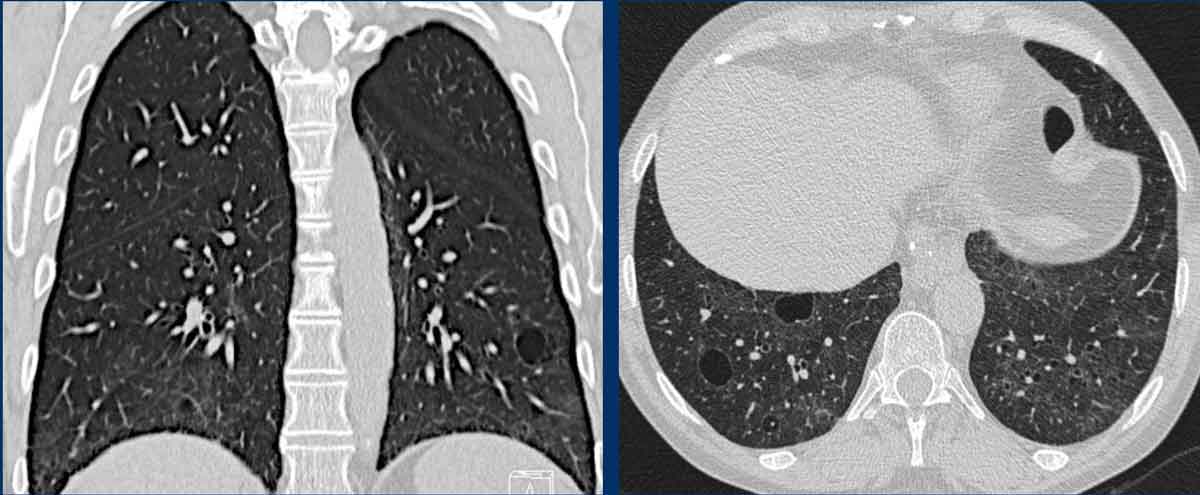
These images are of a 60-year-old man with transitional cell carcinoma.
Study the image.
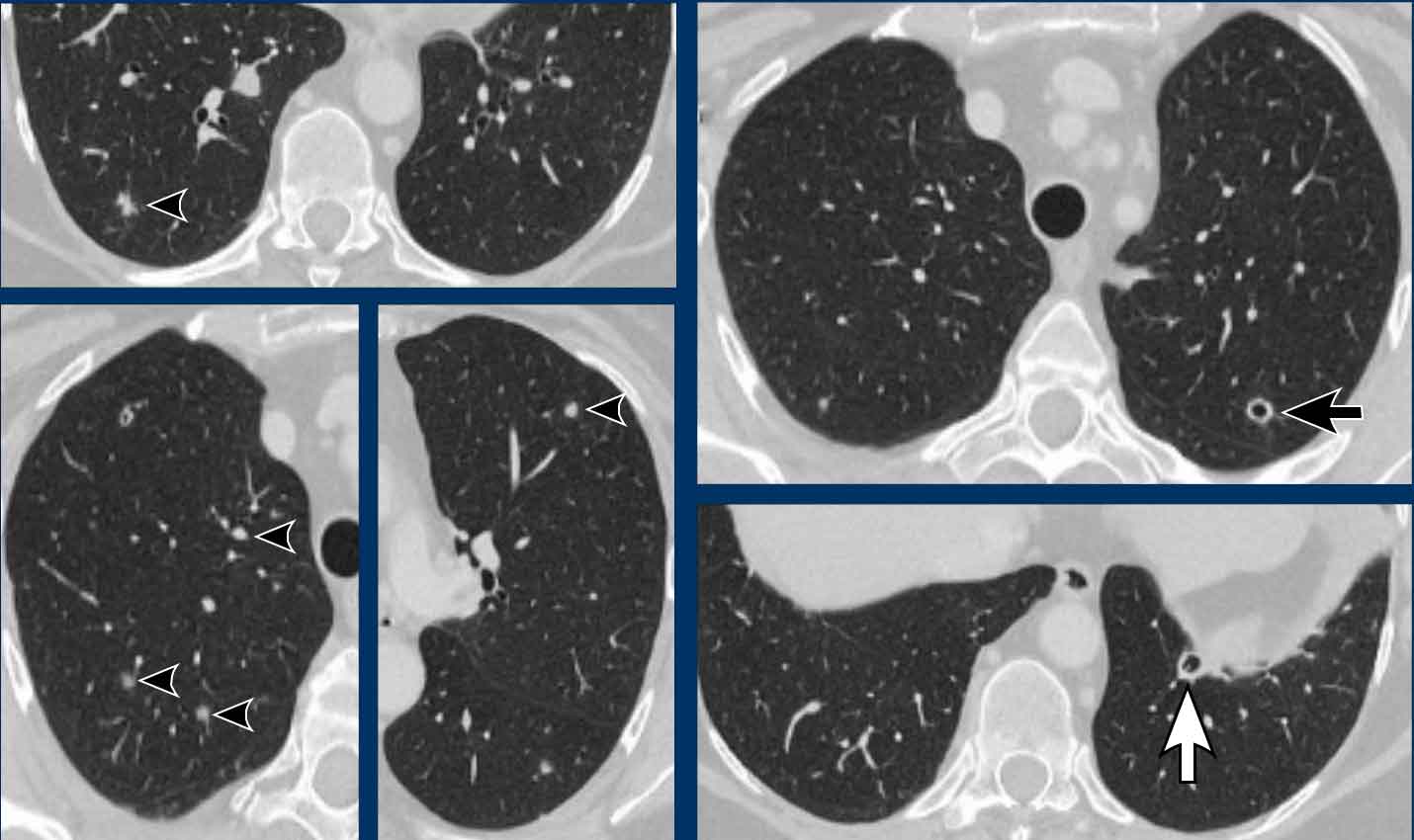
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
There are multiple nodules (arrowheads) and some of them show cavitation (black arrow), which gives them the appearance of thick-walled cysts.
Discussion
In this case there are also lesions in the pleural sinuses and these were metastases.
During follow up these cystic metastases enlarged.
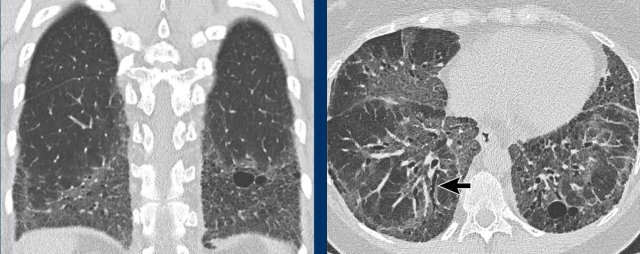
Case 11
These images are of a 55-year-old man with dyspnoe.
There is a history of mixed connective tissue disease (MCTD) and he does not smoke.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
The most characteristic finding is the combination of cysts and ground glass.
Discussion
The most likely diagnosis based on the findings is LIP. The history of MCTD is also helpful.
The diagnosis of DIP is unlikely, since the patient does not smoke and in DIP all the cysts must be localized within an area of ground glass. Here one of the cysts is clearly located within an area of normal lung tissue (arrow).
Case 12
These images are of a 34-year-old man with acute renal insufficiency and dyspnoe.
Study the image.
What is the most characteristic finding?
What is the most likely diagnosis?
Findings
The most characteristic finding is the combination of cysts and ground glass.
Continue...
Discussion
LIP is less likely as the ground glass pattern is far too widespread. In LIP usually there is only a limited area of ground glass in the lower lung fields.
PCP is another possibility, but is also less likely since the cysts are quite large.
In such a case we should also consider the uncommon cases.
In a patient with acute renal insufficiency we should also consider the diagnosis light chain deposition disease (LCDD).
Later this patient proved to be HIV-positive .
A renal biopsy was performed and showed diabetic nephropathy.
Until that moment this patient was not known to have diabetes.
Our final differential diagnosis was LIP or LCDD.
Case 13
These images demonstrate the findings in a patient with light chain deposition disease (LCDD).
Typically the walls show nodular thickenings.
In LCDD usually the kidneys are involved and only in a minority of cases also the lungs.
LCDD is seen frequently as a complication of lymphoproliferative diseases or as a precursor of multiple myeloma.
Case 14
These images are of a 39-year-old woman with dyspnoe.
Study the image.
Are these cysts or mimickers? Is this an incidental finding or do you think it is a cystic lung disease.
What is the most likely diagnosis?
Findings
There are multiple thin-walled cysts. Notice that the cysts are evenly spread throughout the lungs.
Discussion
The pleural sinuses are also involved (arrows).
This means that we can skip diagnoses like LCH and emphysema.
In general, the presence of only simple cysts - regardless of number - should lead to a diagnosis of LAM, except in men when LCH should be diagnosed.
Case 15
These images are of a 65-year-old woman with dyspnoe and a history of smoking.
Study the image.
Are these cysts or mimickers?
What is the most likely diagnosis?
Findings
There are thin-walled cysts in areas of ground glass and fibrosis.
Notice the traction bronchiectasis (arrow).
Continue...
Discussion
The main differential diagnosis of lungcysts in combination with ground glass is DIP, PCP and LIP.
The most likely diagnosis is DIP, becuase the patient is a smoker and because the cysts are only located in areas with ground glass.
DIP cysts are located in the periphery of the lower lung fields and frequently combined with fibrosis.
Case 16
These images are of a 55-year-old man, who presents with dyspnoe and coughing. He has a parrot and does not smoke.
Study the image.
What is the most likely diagnosis?
Findings
There are a few thin-walled cysts in areas with ground glass.
Discussion
The main differential diagnosis of lungcysts in combination with ground glass is DIP, PCP and LIP. However when someone has a parrot, you might also consider hypersensitivity pneumonitis.
And although it is very uncommon, this proved to be hypersensitivity pneumonitis.
Case 17
These images are of a 46-year-old woman.
She has a history of hysterectomy and at physical examination she has a struma.
She does not smoke.
Study the image.
What is the most likely diagnosis?
Findings
There are a few thin-walled cysts in combination with nodules (white arrow) and cavitating nodules also called cheerio sign (black arrow).
Do you need more imaging information?
Discussion
As always we want to have a good look at the pleural sinus.
We can skip the diagnosis LCH, because the pleural sinuses are not involved.
In a non-smoker this diagnosis was already unlikely.
High in the differential diagnosis is metastatic disease.
However no malignancy was found.
This proved to be benign metastatic leiomyoma.
Benign metastasizing leiomyoma is a rare disorder that affects women with a history of uterine leiomyoma, which is found to metastasize most commonly to the lungs, where it presents with nodules, that sometimes cavitate and form cysts.
Charity
All the profits of the Radiology Assistant go to Medical Action Myanmar which is run by Dr. Nini Tun and Dr. Frank Smithuis sr, who is a professor at Oxford university and happens to be the brother of Robin Smithuis.
Click here to watch the video of Medical Action Myanmar and if you like the Radiology Assistant, please support Medical Action Myanmar with a small gift.